Many individuals considering a tummy tuck, or abdominoplasty, often wonder about the financial implications and whether medical insurance will cover the procedure. Tummy tucks are cosmetic surgeries designed to remove excess skin and fat from the abdomen and tighten the abdominal muscles, resulting in a smoother and firmer appearance. The cost of such procedures can vary significantly depending on the surgeon's fees, the geographic location, and the extent of the surgery. Understanding the insurance coverage for a tummy tuck is crucial for those seeking to make an informed decision about their surgical options. This paragraph will explore the factors that determine insurance coverage for tummy tucks and provide insights into the potential financial considerations for individuals interested in this cosmetic procedure.
What You'll Learn
- Eligibility Criteria: Understand who qualifies for insurance coverage
- Policy Details: Check insurance policies for tummy tuck coverage
- Medical Necessity: Determine if a tummy tuck is deemed medically necessary
- Cost Considerations: Explore insurance coverage for procedure costs
- Pre-Approval Process: Learn about insurance pre-approval requirements for tummy tucks

Eligibility Criteria: Understand who qualifies for insurance coverage
When considering insurance coverage for a tummy tuck (also known as abdominoplasty), it's important to understand the eligibility criteria that insurance companies typically use to determine whether a procedure is covered. These criteria often revolve around the medical necessity and the patient's overall health. Here's a detailed breakdown:
Medical Necessity: Insurance companies generally require a strong medical reason for covering a procedure. For a tummy tuck, this could include conditions such as significant skin sagging, excess fat deposits, or muscle separation that has developed after pregnancy or significant weight loss. These issues should be causing functional or aesthetic distress, impacting the individual's quality of life. For example, if a patient has severe diastasis recti (abdominal muscle separation) that is causing chronic back pain and affecting their daily activities, this could be a valid reason for insurance coverage.
Health and Lifestyle Factors: Insurance providers also consider the patient's overall health and lifestyle. They may assess whether the patient has made reasonable efforts to address the issue through non-surgical means. This could include diet, exercise, or weight management programs. If a patient has tried these approaches without success and the condition persists, it strengthens the case for insurance coverage. Additionally, insurance companies might consider factors like age, as older patients may have a higher risk of complications from surgery.
Pre-existing Conditions: Certain pre-existing medical conditions might affect eligibility. For instance, patients with severe cardiovascular issues or diabetes may face additional scrutiny. Insurance companies will assess the patient's ability to undergo surgery safely and recover effectively. In some cases, they may require additional medical assessments or consultations to determine eligibility.
Documentation and Evidence: To support a claim for insurance coverage, patients should be prepared to provide comprehensive documentation. This includes medical records, consultations with specialists, and evidence of previous attempts at non-surgical solutions. The more detailed and organized this documentation, the stronger the case for insurance coverage. It's essential to work closely with healthcare providers to ensure all relevant information is included.
Understanding these eligibility criteria is crucial for patients seeking insurance coverage for a tummy tuck. It empowers individuals to have informed discussions with their healthcare providers and insurance companies, increasing the chances of a successful claim.
Employer Flexibility in Medical Insurance Contributions: Exploring Options
You may want to see also

Policy Details: Check insurance policies for tummy tuck coverage
When considering a tummy tuck (also known as abdominoplasty), it's important to understand the potential coverage provided by your medical insurance. While cosmetic procedures are generally not covered by standard health insurance plans, there are some factors to consider that might influence your insurance coverage.
Review Your Policy Documents: Start by thoroughly reviewing your insurance policy documents. These documents often provide detailed information about what is covered and what is not. Look for sections related to surgical procedures, cosmetic treatments, or elective surgeries. Check if there are any specific exclusions or inclusions related to body contouring or aesthetic surgeries.
Contact Your Insurance Provider: If you cannot find the necessary information in your policy documents, it's crucial to reach out to your insurance provider directly. Contact their customer service or claims department and inquire about tummy tuck coverage. Provide them with details about the procedure you are considering and ask about the potential for coverage. Insurance providers can offer the most accurate and up-to-date information regarding your specific policy.
Understand the Criteria for Coverage: Insurance companies often have specific criteria that must be met for a procedure to be considered covered. These criteria may include the medical necessity of the surgery, the severity of the condition being treated, and the patient's overall health. For a tummy tuck, the insurance provider might require evidence that the procedure is necessary to address a medical issue, such as significant skin sagging or abdominal separation, rather than purely cosmetic concerns.
Explore Additional Benefits: In some cases, insurance plans may offer additional benefits or discounts for specific procedures. Check if your insurance provider has any partnerships or agreements with medical facilities or surgeons that could result in reduced costs or special coverage arrangements. These partnerships can sometimes provide coverage for procedures that might otherwise be considered non-covered.
Remember, while medical insurance may not typically cover the entire cost of a tummy tuck, understanding the details of your policy and exploring all available options can help you make informed decisions about your healthcare and financial planning.
Understanding the Duration of Individual Medical Expense Insurance
You may want to see also

Medical Necessity: Determine if a tummy tuck is deemed medically necessary
When considering a tummy tuck (also known as abdominoplasty) from a medical necessity perspective, it's important to understand the criteria that insurance companies typically use to determine coverage. The primary focus is on whether the procedure is deemed essential for the patient's health and well-being. Here's a step-by-step guide to help you understand this process:
- Health Conditions and Risks: Insurance providers often look for underlying health issues that may benefit from a tummy tuck. For example, individuals with significant abdominal skin sagging and stretch marks resulting from pregnancy, significant weight loss, or genetic factors may be considered for coverage. Additionally, conditions like diastasis recti (separation of abdominal muscles) can be a valid medical reason for the procedure. It is crucial to document and provide medical evidence of such conditions to support the claim.
- Consultation and Medical Opinion: Obtaining a detailed medical opinion from a qualified plastic surgeon or a physician is essential. They should assess the patient's overall health, review medical history, and provide a comprehensive report on the necessity of the tummy tuck. This report should include the patient's specific concerns, the potential risks and benefits, and an explanation of why alternative treatments or non-surgical options are insufficient.
- Pre-existing Conditions: Insurance companies may also consider pre-existing medical conditions that could be exacerbated by the patient's current body shape or size. For instance, individuals with back pain or chronic skin irritation due to loose skin might be eligible for coverage. It is important to provide medical documentation linking these conditions to the need for a tummy tuck.
- Surgical Indications: The procedure should address a significant medical issue or improve the patient's quality of life. Common surgical indications include correcting skin excess, tightening abdominal muscles, and improving body contour. Insurance companies may require evidence of these issues, such as medical notes, photographs, or consultations with specialists.
- Alternative Treatment Options: Insurance adjusters will often explore alternative treatments or non-surgical approaches to determine if a tummy tuck is truly necessary. This may include weight loss programs, exercise regimens, or skin tightening treatments. Patients should be prepared to provide evidence that these options have been exhausted or are not suitable for their specific case.
In summary, establishing medical necessity for a tummy tuck involves a thorough evaluation of the patient's health, a detailed medical opinion, and providing evidence that the procedure is essential for addressing specific health concerns or improving overall well-being. It is a complex process, and patients should be prepared to provide comprehensive documentation to support their case for insurance coverage.
Unraveling the Mystery: What is Medical Bridge Insurance?
You may want to see also

Cost Considerations: Explore insurance coverage for procedure costs
When considering a tummy tuck (also known as abdominoplasty), it's essential to explore the financial aspects and understand the potential coverage provided by medical insurance. While a tummy tuck is a cosmetic procedure, insurance coverage for such treatments can vary widely, and it's crucial to know what your policy entails.
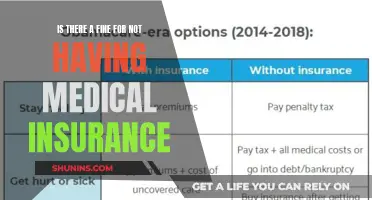
The cost of a tummy tuck can be substantial, often ranging from $5,000 to $15,000 or more, depending on various factors such as the surgeon's fees, the geographic location, the extent of the surgery, and any additional procedures included. These procedures are typically considered elective and are not usually covered by standard medical insurance plans. Insurance companies generally do not provide coverage for cosmetic surgeries unless they are deemed medically necessary to treat a specific condition or to correct a congenital issue.
To determine insurance coverage, you should start by reviewing your policy documents. Contact your insurance provider and inquire about their policies regarding cosmetic procedures. Many insurance companies have specific guidelines and criteria for covering such treatments. Some may cover a portion of the cost if the procedure is deemed necessary to improve a medical condition, such as severe skin sagging after significant weight loss or post-pregnancy abdominal separation. In such cases, the insurance might cover the surgical portion but not the aesthetic enhancements.
It's important to note that insurance coverage for tummy tucks is often limited and may require a detailed explanation of the medical necessity. The insurance company will likely require medical documentation and an assessment by a qualified physician to determine if the procedure is appropriate and necessary. This process can be complex and may involve multiple consultations and medical reports.
Additionally, some insurance providers offer specialized plans or packages that include cosmetic procedures, providing coverage under certain conditions. These plans might be more comprehensive and could offer better coverage for tummy tucks. Exploring these options and understanding the terms and conditions can be beneficial for those considering such procedures.
In summary, while medical insurance may not typically cover the full cost of a tummy tuck, there are avenues to explore. Reviewing your insurance policy, understanding the coverage criteria, and seeking professional medical advice can help you navigate the financial considerations associated with this cosmetic procedure.
Life Insurance and Medicaid: Navigating Dual Coverage
You may want to see also

Pre-Approval Process: Learn about insurance pre-approval requirements for tummy tucks
The pre-approval process for insurance coverage of a tummy tuck, also known as abdominoplasty, can vary depending on your insurance provider and the specific policies they offer. It is essential to understand these requirements to ensure a smooth and successful approval process. Here's a detailed guide to help you navigate this step:
Understand Your Insurance Plan: Begin by thoroughly reviewing your medical insurance policy. Contact your insurance provider and inquire about their coverage for cosmetic procedures, including tummy tucks. Ask about any specific guidelines or criteria they use to determine eligibility for coverage. Understanding the basics of your plan will help you anticipate potential challenges and requirements.
Research and Gather Information: Conduct thorough research on the insurance pre-approval process for tummy tucks. Many insurance companies have specific requirements and forms that need to be completed before they can consider a procedure for coverage. Look for online resources, medical websites, or forums where you can find information on insurance pre-approval. This research will provide you with a better understanding of the necessary steps and potential challenges.
Consult Your Surgeon: Schedule a consultation with a board-certified plastic surgeon who specializes in tummy tucks. Discuss your insurance coverage and the pre-approval process with them. They can provide valuable insights and may have experience navigating the insurance system. Your surgeon can also help you understand the medical necessity of the procedure and provide the necessary documentation to support your case.
Complete Required Documentation: Insurance companies often require a comprehensive medical history and justification for the procedure. Gather all relevant medical records, including any previous surgeries, medical conditions, and treatment plans. Your surgeon will likely provide specific forms and guidelines to ensure the documentation meets the insurance company's standards. Be thorough and accurate in your submissions to increase the chances of a successful pre-approval.
Submit the Application: Once you have gathered all the necessary information and completed the required documentation, submit your application to your insurance provider. Follow their instructions carefully and ensure that all forms are filled out correctly. Provide any additional information or medical opinions that support the need for a tummy tuck. The insurance company will review your application and may require further clarification or additional medical opinions.
Remember, the pre-approval process can take time, and it is essential to start this process well in advance of your desired surgery date. Being proactive and thorough in your approach will increase the likelihood of a positive outcome. Always keep detailed records of all communications and documentation to ensure a smooth and efficient process.
Dental Implants: Unlocking Coverage Secrets with Medical Insurance
You may want to see also
Frequently asked questions
In most cases, medical insurance does not cover cosmetic procedures like a tummy tuck, as they are considered elective surgeries. These procedures are often deemed "cosmetic" and not "medically necessary," which means insurance companies generally do not provide coverage for such treatments.
There might be rare instances where insurance could consider a tummy tuck as a covered procedure. This could occur if the surgery is deemed necessary for medical reasons, such as reconstructing skin after significant weight loss or correcting a hernia. However, this is uncommon and usually requires a thorough evaluation by the insurance provider.
Absolutely! Many cosmetic surgery clinics offer financing plans or work with medical financing companies to help patients manage the costs. These options can provide a way to afford the procedure without relying solely on insurance coverage. It's best to discuss these alternatives with the surgical practice to understand the available options.