The debate surrounding the relationship between Medicaid and employer-sponsored insurance is a complex one. While some argue that Medicaid serves as a primary safety net for those who cannot afford employer coverage, others suggest that it acts as a secondary option, providing coverage for those who have already exhausted their employer benefits. This discussion is crucial in understanding the healthcare landscape and the accessibility of healthcare for different segments of the population.
What You'll Learn
- Eligibility: Medicaid eligibility criteria and income thresholds
- Coverage Prioritization: Determining primary and secondary insurance coverage
- Coordination: Managing claims and payments between Medicaid and employer insurance
- Cost Sharing: Understanding copayments, deductibles, and out-of-pocket expenses
- Transition Periods: Smooth transitions between different insurance coverage

Eligibility: Medicaid eligibility criteria and income thresholds
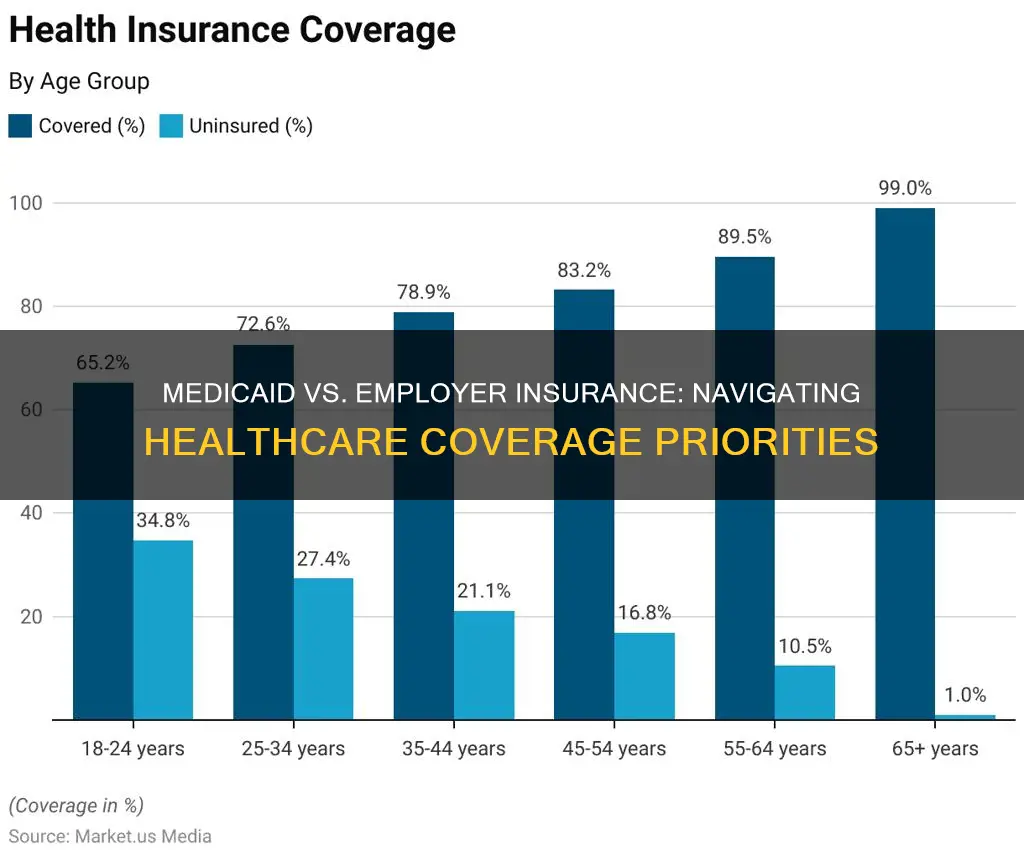
Medicaid eligibility is primarily based on income and asset levels, ensuring that those with limited financial resources can access essential healthcare services. The specific criteria and income thresholds vary by state, as Medicaid is a joint federal-state program. Generally, eligibility is determined by comparing a household's income to the federal poverty level (FPL), which is adjusted annually. For instance, in 2023, the FPL for a family of three is set at $23,520, and for a family of four, it is $31,700. States may also consider other factors, such as pregnancy, disability, or being over 65 years old, to expand eligibility beyond these income thresholds.
Income thresholds are designed to ensure that Medicaid benefits are provided to those who need them most. Households with incomes below the FPL threshold are typically eligible for full Medicaid coverage, including medical assistance and long-term care services. For those with incomes above the FPL but below the state-set threshold, they may be eligible for partial coverage, often referred to as 'Medicaid expansion' programs. These programs aim to provide healthcare coverage to low-income individuals who do not qualify for full Medicaid but still struggle financially.
The income eligibility criteria for Medicaid can be complex, especially for families with varying income sources. For instance, in some states, income is calculated based on the previous month's earnings, while in others, it may be based on the previous year's income. Additionally, certain assets, such as a primary residence, vehicle, or personal belongings, are often exempt and do not affect eligibility. However, other assets, like bank accounts or investments, may be considered in determining eligibility, especially for long-term care services.
It is important to note that Medicaid eligibility rules can change, and states have the flexibility to set their own criteria. Therefore, individuals should refer to their state's Medicaid website or contact their local Medicaid office for the most accurate and up-to-date information regarding eligibility and income thresholds. Understanding these criteria is crucial for those seeking healthcare coverage and ensuring they meet the necessary requirements to access Medicaid benefits.
In summary, Medicaid eligibility is primarily income-based, with states setting their own thresholds. Understanding these criteria is essential for individuals to determine their eligibility and access the healthcare they need. By staying informed about the specific rules in their state, individuals can navigate the Medicaid system effectively and take advantage of the financial assistance available to them.
Oral Surgery and Insurance: Navigating Coverage and Costs
You may want to see also

Coverage Prioritization: Determining primary and secondary insurance coverage
When it comes to insurance coverage, prioritizing the primary and secondary insurance providers is crucial to ensure that individuals receive the necessary medical care without incurring excessive financial burdens. This process, known as coverage prioritization, is particularly important when an individual has both public and private insurance options available. In the context of Medicaid and employer-sponsored insurance, understanding the hierarchy of coverage is essential.
Medicaid, a joint federal and state program, is designed to provide healthcare coverage to low-income individuals and families. It is a safety net for those who may not qualify for private insurance or have limited financial resources. On the other hand, employer-sponsored insurance is typically a private health insurance plan offered by an employer to their employees. This type of insurance often provides comprehensive coverage, including hospitalization, doctor visits, and prescription drugs. When an individual has both Medicaid and employer insurance, the priority of coverage needs to be established.
The general rule is that employer-sponsored insurance is considered the primary insurance, while Medicaid acts as the secondary coverage. This means that the employer insurance plan will typically cover the majority of the individual's medical expenses, and Medicaid will step in to provide additional benefits or cover any remaining costs. This prioritization ensures that the individual's primary source of insurance, which is often more comprehensive and stable, is utilized first. It also prevents the individual from incurring out-of-pocket expenses that might be covered by the secondary insurance, which could be more limited in scope.
Determining the primary and secondary insurance coverage involves a few key considerations. Firstly, the individual's enrollment in both programs is essential. They must be actively enrolled in both Medicaid and employer-sponsored insurance to establish the correct coverage hierarchy. Secondly, understanding the specific benefits and exclusions of each plan is crucial. Some employer plans might have specific provisions that override the general rule, such as offering limited coverage for certain medical services, which could make Medicaid the primary insurer in those cases. Lastly, the individual's financial situation and medical needs should be considered. If the individual's employer insurance is insufficient or inadequate, Medicaid can provide the necessary coverage to ensure access to healthcare.
In summary, coverage prioritization is a critical aspect of managing insurance benefits. When dealing with Medicaid and employer insurance, the general principle is that employer-sponsored insurance takes precedence. However, this may vary based on individual circumstances, and a thorough understanding of the plans' provisions is essential to ensure that individuals receive the appropriate level of coverage. This process helps individuals navigate the complexities of healthcare financing and ensures they have access to the care they need while minimizing financial strain.
Understanding Dermatologist Coverage: Unlocking Insurance Benefits for Skin Health
You may want to see also

Coordination: Managing claims and payments between Medicaid and employer insurance
Medicaid and employer-based insurance are two distinct public and private health coverage programs, respectively, and their coordination is crucial to ensure that individuals receive the healthcare they need without unnecessary gaps in coverage. When an individual has both Medicaid and employer insurance, the coordination of these programs becomes essential to manage claims and payments effectively.
The primary goal of coordination is to prevent double-dipping, where an individual receives benefits from both programs for the same medical service, which can lead to financial inefficiencies and potential fraud. When an individual is enrolled in both Medicaid and employer insurance, the coordination process involves determining the primary payer for specific medical services. Typically, Medicaid is considered the primary payer, especially for low-income individuals who may not have comprehensive employer coverage. This means that Medicaid will cover the eligible medical expenses first, and any remaining costs will be the responsibility of the employer insurance.
The coordination process typically involves a few key steps. Firstly, the individual's healthcare provider or the billing department must submit a claim to both Medicaid and the employer insurance plan. The claim should detail the medical services provided, the costs incurred, and the patient's insurance information. Medicaid has its own claims processing system, and it will review the claim to determine eligibility and coverage. Simultaneously, the employer insurance plan will also process the claim, verifying the individual's enrollment and the specific coverage provided by the plan.
Once the claims are processed, the coordination process comes into play. Medicaid will pay for the eligible services first, and the remaining costs will be billed to the employer insurance. This ensures that the individual receives the necessary healthcare without incurring excessive out-of-pocket expenses. The employer insurance plan will then coordinate with the healthcare provider to settle the remaining costs, providing coverage for services that Medicaid did not cover. Effective coordination requires clear communication and cooperation between the Medicaid agency, employer insurance carriers, healthcare providers, and, most importantly, the individuals enrolled in both programs.
In summary, managing claims and payments between Medicaid and employer insurance is a complex but essential process to ensure seamless healthcare coverage. It involves determining primary payer status, submitting claims to both programs, and coordinating payments to avoid financial overlaps. By streamlining this coordination, individuals can access the healthcare they need without facing barriers or delays, ultimately improving their overall healthcare experience.
Navigating Florida's Medicaid: Unlocking the Best Coverage Options
You may want to see also

Cost Sharing: Understanding copayments, deductibles, and out-of-pocket expenses
Medicaid and employer-based insurance are two distinct healthcare coverage options, and understanding their relationship is crucial for individuals seeking affordable and comprehensive healthcare. When it comes to cost-sharing mechanisms, both programs have their own unique approaches to managing expenses.
Copayments: These are fixed amounts that individuals pay for specific healthcare services, such as a doctor's visit or a prescription. Copayments are typically lower for primary care services and may be waived for certain preventive care, as mandated by the Affordable Care Act. In Medicaid, copayments are generally minimal or non-existent, ensuring that low-income individuals can access necessary medical services without incurring significant financial burdens. On the other hand, employer insurance plans often include copayments, which can vary depending on the plan's structure and the type of service. For instance, a copayment might be required for a specialist visit or a specific procedure.
Deductibles: This is the amount of money an individual must pay out of pocket before their insurance coverage kicks in. Deductibles are usually higher for employer-based plans, and they can vary widely depending on the plan's design. For instance, a high-deductible health plan (HDHP) often has a lower monthly premium but requires the individual to pay a higher deductible before receiving comprehensive coverage. In contrast, Medicaid programs typically have lower or no deductibles, making it more accessible to those with limited financial resources. When an individual meets their deductible, they become eligible for the full range of benefits covered by their insurance.
The concept of out-of-pocket expenses is essential to understand as it represents the total amount an individual pays for healthcare services before their insurance coverage begins. This includes copayments, deductibles, and other costs like coinsurance (a percentage of the total cost of a service). In Medicaid, out-of-pocket expenses are minimized to ensure that beneficiaries can access necessary care without facing financial barriers. For employer insurance, out-of-pocket expenses can vary significantly depending on the plan's specifics. Some plans may have lower out-of-pocket costs for in-network providers, while others might require higher payments for out-of-network services.
Understanding these cost-sharing elements is vital for individuals to navigate the healthcare system effectively. Medicaid's approach to cost-sharing aims to provide essential healthcare services to those in need, while employer insurance plans often offer more comprehensive coverage with varying levels of cost-sharing. When considering insurance options, individuals should carefully review the details of each plan to ensure they understand their financial responsibilities and the extent of their coverage.
Medicaid and Private Insurance: A Dual Coverage Guide for Ohio Residents
You may want to see also

Transition Periods: Smooth transitions between different insurance coverage
When individuals or families are transitioning between different insurance plans, such as moving from one employer's insurance to another or transitioning from private insurance to Medicaid, it is crucial to ensure a smooth and seamless process. This is especially important to avoid any gaps in coverage, which could lead to financial strain and potential health risks. Here are some strategies to facilitate these transitions:
Review and Understand Policies: Before the transition, thoroughly review the policies of both the current and future insurance providers. Understand the coverage details, including any exclusions, limitations, and benefits. This knowledge will help individuals make informed decisions and ensure they are aware of what services are covered during the transition period. For instance, if someone is moving from a private plan to Medicaid, they should be aware of the potential changes in coverage and any additional resources they might need to access healthcare services.
Coordinate with Insurance Companies: Effective communication between the individual, the current insurance provider, and the future insurance company is essential. Inform the current insurer about the upcoming change and request their assistance in ensuring a smooth transition. They might provide guidance on the necessary steps, such as updating records, transferring benefits, or providing temporary coverage to avoid any lapse in insurance. Similarly, the future insurance provider should be contacted to understand their process for onboarding new members and any specific requirements they need from the individual.
Enroll in Temporary Coverage (if necessary): In some cases, there might be a gap between the end of one policy and the start of another. During this transition period, individuals can consider enrolling in temporary health insurance to maintain coverage. This could be a short-term plan or a bridge policy offered by the current insurer or a marketplace option. By doing so, they can ensure that their healthcare needs are met without any interruption, especially if they have pre-existing conditions or require immediate medical attention.
Update Personal and Medical Information: During the transition, it is vital to keep all personal and medical information up-to-date. This includes providing accurate and current details to both insurance companies. Ensure that your contact information, address, and any relevant medical history are shared with the new insurer. This step is crucial for accurate billing, claims processing, and providing the best possible care during the transition.
Seek Assistance from Healthcare Providers: Healthcare professionals can play a significant role in guiding individuals through these transitions. They can help patients understand their options, provide referrals to suitable insurance plans, and offer advice on managing healthcare during the transition. Additionally, providers can assist in coordinating care, especially if the individual has specific medical needs that require specialized attention.
Envita Medical Center: Insurance Coverage Explained
You may want to see also
Frequently asked questions
Medicaid is a government-funded health insurance program designed to provide coverage to low-income individuals and families. It is a primary source of health insurance for many vulnerable populations. On the other hand, employer-sponsored insurance is provided by an employer and is typically a secondary or supplementary insurance option for employees.
Yes, it is possible for an individual to be enrolled in both Medicaid and have employer-sponsored insurance. In such cases, the employer's insurance may cover certain medical expenses, while Medicaid provides coverage for the remaining costs. This dual coverage can ensure comprehensive healthcare benefits for the individual.
When an individual has both Medicaid and employer insurance, the priority of coverage is determined by specific rules. Generally, employer insurance is considered the primary coverage, and Medicaid becomes the secondary payer. This means that the employer's insurance will be utilized first, and any remaining eligible expenses will then be covered by Medicaid.