Medicaid is a federal and state-funded health insurance program that provides coverage to low-income individuals and families. While Medicaid is primarily designed to serve those who meet specific income and asset requirements, it can also be used as a secondary insurance policy. This means that individuals with other primary insurance coverage, such as private health insurance, can still qualify for Medicaid and receive additional benefits. Having Medicaid as a secondary insurance can help cover gaps in coverage, provide financial assistance for medical expenses, and ensure that individuals have access to necessary healthcare services. Understanding the eligibility criteria and how Medicaid can complement other insurance plans is essential for those seeking comprehensive healthcare coverage.
What You'll Learn

Medicaid Coverage: Understanding eligibility and benefits
Medicaid is a joint federal and state program that provides health coverage for individuals and families with low incomes and resources. It is designed to offer essential healthcare services to those who might not otherwise be able to afford them. One common question regarding Medicaid is whether it can be considered as secondary insurance. The answer is yes; Medicaid can indeed function as a secondary payer in certain situations.
When an individual has both private insurance and Medicaid, the private insurance typically serves as the primary payer for covered services. Medicaid, in this case, becomes the secondary payer, stepping in to cover any remaining costs that the primary insurance doesn't. This arrangement ensures that individuals receive the necessary medical care while also utilizing their private insurance benefits. It's important to note that the specific rules and regulations regarding secondary payer status can vary by state, so it's essential to check your state's Medicaid guidelines.
Eligibility for Medicaid is based on income and resource limits, which are determined by the federal poverty level. These guidelines are adjusted annually to account for inflation. Individuals and families with incomes below the federal poverty threshold may qualify for full Medicaid coverage, including medical services, hospitalization, and long-term care. The program also covers pregnant women, children, the elderly, and individuals with disabilities, ensuring that vulnerable populations have access to essential healthcare.
Medicaid coverage offers a wide range of benefits, including doctor visits, hospital stays, emergency services, prescription drugs, and mental health care. The specific services covered may vary depending on the state and the individual's eligibility category. For example, pregnant women might receive prenatal care and postpartum services, while children may have access to well-child visits and immunizations. Understanding your state's Medicaid program and its benefits is crucial to ensure you receive the healthcare you need.
In summary, Medicaid can indeed be considered as secondary insurance when an individual has both private coverage and Medicaid. This arrangement allows for a seamless integration of benefits, ensuring that individuals receive the necessary medical care. Medicaid's eligibility criteria and benefits vary by state, so it is essential to explore your state's specific guidelines to understand your coverage options and ensure you receive the healthcare you deserve.
Understanding Medical Insurance: The Three Essential Coverages Explained
You may want to see also

Secondary Insurance: How it works with Medicaid
Secondary insurance, when combined with Medicaid, can be a powerful tool for managing healthcare costs and ensuring comprehensive coverage. This arrangement allows individuals to have multiple insurance plans, with one acting as the primary and the other as the secondary. When it comes to Medicaid, understanding how secondary insurance works is crucial for maximizing benefits and minimizing out-of-pocket expenses.
Medicaid, a joint federal and state program, provides essential healthcare coverage to low-income individuals and families. It offers a range of benefits, including doctor visits, hospital stays, and prescription drug coverage. However, Medicaid's coverage can sometimes be limited, and this is where secondary insurance comes into play. Secondary insurance acts as a supplement, filling in the gaps where Medicaid might fall short. For instance, if a person with Medicaid requires specialized medical care that is not covered by Medicaid, their secondary insurance plan could step in to cover the remaining costs.
The process typically involves coordination between the primary and secondary insurance providers. When a Medicaid recipient receives medical services, the primary responsibility is for the Medicaid plan to cover the eligible expenses. However, if the services exceed Medicaid's coverage or if there are specific treatments or medications not covered by Medicaid, the secondary insurance plan will step in to cover the remaining amount. This ensures that individuals receive the necessary care without facing significant financial burdens.
It's important to note that not all insurance plans are eligible to be secondary to Medicaid. The secondary insurance must be a comprehensive health plan that provides coverage for a wide range of medical services. Additionally, the secondary plan should have a network of healthcare providers that includes Medicaid-participating providers to ensure smooth and efficient claims processing.
When considering secondary insurance with Medicaid, individuals should carefully review their Medicaid plan's guidelines and understand the specific terms and conditions of their secondary insurance policy. This includes knowing the coverage limits, exclusions, and any pre-authorization requirements. Proper coordination and communication between healthcare providers and insurance companies are essential to ensure that claims are processed efficiently and that individuals receive the full benefits of both their primary and secondary insurance plans.
Navigating Surrogacy Costs: Unlocking Medical Insurance Coverage
You may want to see also

Coordination of Benefits: Managing dual insurance claims
The concept of 'Coordination of Benefits' (COB) is crucial when individuals have multiple insurance plans, especially when one of them is a government-funded program like Medicaid. COB ensures that when an individual files a claim, the insurance companies involved work together to minimize duplication of benefits and ensure fair compensation. This process is particularly important for those with Medicaid as secondary insurance, as it can help manage costs and streamline the claims process.
When an individual has both private insurance and Medicaid, the insurance companies must coordinate to determine which plan will cover specific services. The primary insurance plan, usually the one with the highest coverage, will be responsible for paying the majority of the claim. Medicaid, as the secondary insurance, will then step in to cover any remaining costs, ensuring that the individual receives the necessary medical care without incurring excessive expenses. This coordination prevents individuals from being overcharged and helps maintain a balanced financial relationship between the insurance providers.
The process of COB typically involves the following steps: First, the individual files a claim with their primary insurance provider, providing details of the medical service or treatment received. The primary insurer then reviews the claim and determines the extent of coverage. If the primary insurance plan covers the service, it processes the claim and pays the provider directly. Simultaneously, the secondary insurance, in this case, Medicaid, is notified of the claim to ensure it is aware of the individual's coverage.
Medicaid's role in COB is to verify the individual's eligibility and ensure that the services provided are within the scope of its coverage. It then pays its portion of the claim directly to the healthcare provider or the primary insurer, depending on the coordination agreement between the two parties. This streamlined process ensures that the individual receives the necessary medical attention without the hassle of multiple payments or claims.
Effective COB management is essential to maintain a positive relationship between insurance providers and policyholders. It prevents confusion, reduces administrative costs, and ensures that individuals receive the full benefit of their insurance coverage. When dealing with dual insurance plans, such as Medicaid and private insurance, proper coordination can lead to a more efficient and cost-effective healthcare system for all involved parties.
Medicaid's Role in Copay Coverage: Navigating Insurance Complexities
You may want to see also

Medicaid's Role: Ensuring access to healthcare services
Medicaid plays a crucial role in ensuring that individuals and families across the United States have access to essential healthcare services. It is a joint federal and state program designed to provide medical assistance to low-income individuals and families, offering a safety net for those who might otherwise struggle to afford healthcare. The program's primary goal is to ensure that everyone, regardless of their financial situation, can access necessary medical care.
When it comes to the concept of 'secondary insurance,' it refers to a situation where an individual has multiple insurance plans, and one of them is Medicaid. This arrangement is particularly useful for those who have other insurance coverage but still qualify for Medicaid due to their income level. For instance, an individual might have a private employer-sponsored plan but still be eligible for Medicaid, allowing them to utilize the program's benefits as a secondary layer of coverage. This ensures that even with primary insurance, individuals can still access Medicaid's comprehensive benefits when needed.
Medicaid's role in ensuring access to healthcare services is multifaceted. Firstly, it provides coverage for a wide range of medical services, including doctor visits, hospital stays, emergency care, prescription drugs, and more. This comprehensive coverage ensures that individuals can address their medical needs without incurring significant financial burdens. For instance, Medicaid covers routine check-ups and preventive care, which are essential for maintaining good health and managing chronic conditions effectively.
Secondly, Medicaid offers financial protection by covering a significant portion of healthcare costs, often up to 100% for eligible individuals. This means that even for those with primary insurance, Medicaid can step in to cover any remaining costs, ensuring that financial barriers do not prevent access to necessary medical care. This is especially important for low-income families who might otherwise delay or forgo medical treatment due to the high costs associated with healthcare services.
Furthermore, Medicaid's impact extends beyond individual access to healthcare. It plays a vital role in improving community health outcomes. By providing comprehensive coverage, Medicaid ensures that people can manage their health, leading to better disease management and reduced hospital admissions. This, in turn, contributes to a healthier population and lower healthcare costs for society as a whole.
In summary, Medicaid is a critical program that ensures access to healthcare services for millions of Americans. Its role as secondary insurance allows individuals to have additional coverage, ensuring they can access necessary medical care without financial strain. By providing comprehensive benefits and financial protection, Medicaid empowers individuals and communities to take control of their health, ultimately leading to improved overall well-being.
Navigating Medical Insurance Cancellation: Your Workplace Options Explained
You may want to see also

Cost-Sharing: Exploring financial responsibilities with secondary insurance
When considering Medicaid as a secondary insurance option, it's essential to understand the concept of cost-sharing and how it applies to your healthcare coverage. Cost-sharing refers to the financial responsibilities you have when accessing healthcare services, and it can vary depending on your insurance plan and eligibility.
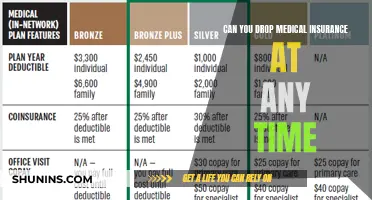
In the context of secondary insurance, such as Medicaid, cost-sharing typically involves copayments, coinsurance, and deductibles. Copayments are fixed amounts you pay at the time of service for specific medical procedures or visits. For example, you might have a copay of $10 for a doctor's visit or $20 for a prescription medication. Coinsurance, on the other hand, is a percentage of the total cost of a covered service that you pay after meeting your deductible. For instance, if a medical procedure costs $100 and your coinsurance rate is 20%, you would pay $20. Deductibles are the amount you must pay out of pocket before your insurance coverage kicks in.
Medicaid, as a government-funded program, often has different cost-sharing requirements compared to private insurance plans. The specific financial responsibilities will depend on your state's Medicaid program and your eligibility category. Some Medicaid beneficiaries may have lower or waived cost-sharing, meaning they pay nothing for covered services. Others might have moderate copayments for certain services, ensuring that healthcare remains accessible and affordable. It's crucial to review your Medicaid benefits and understand the cost-sharing structure to manage your healthcare expenses effectively.
Exploring the cost-sharing aspects of secondary insurance is vital for managing your healthcare finances. Understanding copayments, coinsurance, and deductibles will help you navigate the healthcare system and make informed decisions about your medical care. By knowing your financial responsibilities, you can ensure that you receive the necessary treatment while also being mindful of your out-of-pocket expenses.
Maximize Your Life Insurance: Strategies to Shield from Medicaid
You may want to see also
Frequently asked questions
Yes, it is possible to have both Medicaid and private health insurance simultaneously, with Medicaid serving as the secondary coverage. This arrangement is often referred to as "dual coverage" or "dual eligibility." In this scenario, your private insurance will typically be your primary coverage, and Medicaid will provide additional benefits or cover specific services that your primary insurance may not fully cover.
Eligibility for Medicaid as a secondary insurance option depends on your income and the rules set by your state's Medicaid program. You can contact your local Medicaid office or visit their website to understand the specific requirements. Generally, you'll need to meet the income guidelines and may also need to be a U.S. citizen or legal resident.
Having Medicaid as a secondary insurance can offer several benefits. It can help fill gaps in coverage, especially for prescription drugs, long-term care, or specific medical services that your primary insurance might not fully cover. Medicaid often provides comprehensive coverage, including doctor visits, hospitalization, and preventive care, ensuring that you have access to a wide range of healthcare services.
Most private insurance providers are open to accepting Medicaid as secondary coverage. However, it's essential to review your specific insurance plan and understand the terms and conditions. Some plans might have specific requirements or restrictions regarding secondary insurance. It's advisable to contact your private insurance company to confirm their policies and ensure a smooth coordination of benefits between your primary and secondary insurance providers.