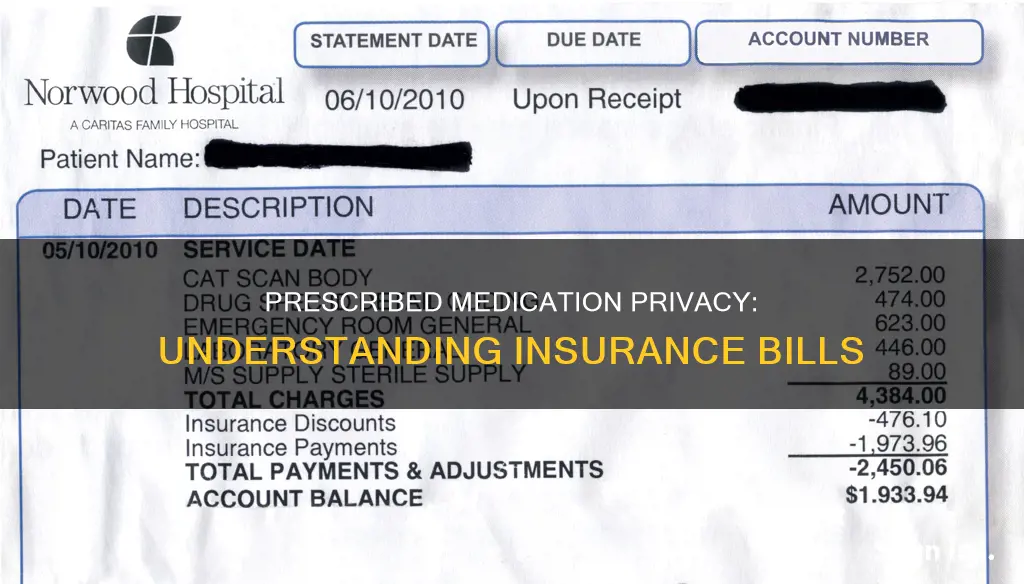
Understanding what your insurance covers and what you must pay for healthcare can be confusing. It is important to know what to expect financially when you need to go to the doctor. After you visit your doctor, your doctor’s office submits a bill (also called a claim) to your insurance company. A claim lists the services your doctor provided to you. The insurance company uses the information in the claim to pay your doctor for those services. When the insurance company pays your doctor, it might send you a report called an Explanation of Benefits, or EOB. This will show you what the insurance company did when it received your doctor’s bill (claim). You need to be able to read and understand the EOB to know what your insurance company is paying for, what it’s not paying for, and why. An EOB is not a bill.
Your doctor’s office might send you a statement. A statement shows how much your doctor’s office billed your insurance company for the services you received. If you receive a statement before your insurance company pays your doctor, you do not need to pay the amounts listed at that time. After your insurance company pays your doctor, you may need to pay the doctor any balance due.
Some insurance companies do send out a list of medications you have filled to the insurance holder. Whether or not prescription drugs will show up on your insurance, and how much information is viewable, will depend on your insurance company.
| Characteristics | Values |
|---|---|
| Do medicines show up on insurance bills? | No |
| Do medicines show up on insurance statements? | No |
| Do insurance companies disclose information about medicines? | Only if requested by the primary care holder |
| Can the primary care holder see the records? | Yes |
| Do all insurance companies send out a list of medications? | No |
| Do some insurance companies send out a list of medications? | Yes |
| Does the list of medications include the name of the drug? | Yes |
| Does the list of medications include the name of the prescriber? | Yes |
| Does the list of medications include the name of the pharmacy? | Yes |
| Does the list of medications include the dosage? | Yes |
| Does the list of medications include the reason for the prescription? | Yes |
What You'll Learn
- Insurance companies may send a list of medications to the insurance holder
- You can check your insurance coverage online or by calling your insurance company
- You can ask your pharmacist if your prescription is covered by your insurance
- If your insurance doesn't cover your medication, you can request an exception
- If you are on your parents' insurance, they may be able to see your prescription records

Insurance companies may send a list of medications to the insurance holder
When it comes to insurance coverage for prescription medications, it's important to understand what your specific plan covers and what you need to pay for. While health insurance can help with the cost of prescription medications, the details of coverage vary across plans.
In general, insurance companies maintain a list of medications that are covered under your plan, known as a "formulary". This list outlines the different tiers of coverage, with lower-tier numbers indicating better coverage and lower out-of-pocket costs for the insured. It is worth noting that insurance plans may have different coverage rules, and obtaining information about medication coverage can sometimes be challenging if you are not a current member of the plan.
Now, regarding the visibility of prescribed medications on insurance bills, it depends on the insurance company. Some insurance companies do send out a list of medications filled under the plan to the insurance holder. This list may include details such as the drug name, prescriber, pharmacy, dosage, route, and reason for prescription. However, not all insurance companies disclose this information unless specifically requested by the primary care holder.
It is always a good idea to review your insurance plan's benefits and limitations, especially when it comes to prescription medication coverage. You can do this by visiting your insurer's website, reviewing the Summary of Benefits and Coverage, or calling your insurer directly. Additionally, most insurance companies provide online portals or mobile apps that can help you understand your coverage and pricing for specific medications.
Term Insurance Takeover: Navigating the Transition When Your Carrier is Sold
You may want to see also

You can check your insurance coverage online or by calling your insurance company
When it comes to checking your insurance coverage, you have a few options available to you. You can either check online or give your insurance company a call.
Checking Insurance Coverage Online
Firstly, you can check your insurance coverage online. Most insurance companies have websites and online portals where you can log in and review your coverage details. To access these, you'll need to create an account using the email address associated with your insurance plan. Once logged in, you can explore the website and online tools to find information about your coverage.
Some insurance companies also offer mobile apps that can help you understand your coverage and pricing for specific drugs. These apps often require you to create an account and log in to access your personalized information.
Additionally, you can refer to your Summary of Benefits and Coverage (SBC). This document outlines the services covered by your plan and provides details about how much you'll pay for each tier of coverage. If you don't have a copy, you can request one from your insurance company or access it through your online account.
Calling Your Insurance Company
Another option is to call your insurance company directly. You can find their phone number on your insurance card, or on their website. When calling, make sure to have the following information ready:
- Your insurance member ID, found on your insurance card.
- The name of the medication and the prescribed dosage.
Once you connect with a representative, provide your account information and ask about the coverage benefits for the medication in question. They will be able to guide you through the details of your coverage and any exceptions or prior authorizations that may be required.
Understanding Your Insurance Coverage
It's important to remember that different insurance plans cover different medications and services. Your doctor also needs to be part of the insurance company's network for your visits to be covered. Understanding your specific plan's benefits, limitations, and network of providers will help you make the most of your insurance coverage.
Understanding the Nuances of S-DVI Insurance: Term or Whole Life?
You may want to see also

You can ask your pharmacist if your prescription is covered by your insurance
If you're at the pharmacy and unsure whether your prescription is covered by your insurance, you can ask the pharmacist. They will be able to tell you if your insurance plan covers the cost of your prescription. If it's not covered, they can also tell you if there are any covered alternatives.
If your insurance plan doesn't cover the cost of your prescription, you can ask your pharmacist or healthcare professional about generic medications or alternative drugs that may have the same effects. Generic medications usually cost less and are more likely to be covered by your insurance.
You can also ask your pharmacist about the possibility of an emergency fill, which would provide you with a short supply of the medication while you wait for approval from your insurance company.
If you're unsure about your insurance coverage, it's best to call the number on the back of your insurance card. When calling, make sure you have your insurance member ID, the name of the medication, and the prescribed dosage.
The Secret Behind LOA in Insurance: Unlocking the Mystery of Loss of Amenity
You may want to see also

If your insurance doesn't cover your medication, you can request an exception
If your insurance doesn't cover your medication, it can be a stressful situation. However, there are a few steps you can take to request an exception and explore alternative options. Here are some detailed instructions to guide you through the process:
Understand the Reason for Denial
Before taking any action, it is essential to understand why your medication isn't covered. Contact your pharmacist or insurance provider to clarify the reason for the denial of coverage. Sometimes, it could be due to a simple mistake or a paperwork issue. Knowing the reason will help you navigate the next steps more effectively.
Ask for an Exception
If your insurance company denies medication coverage, you have the right to request an exception to their formulary, which is their list of covered medications. Your healthcare provider will need to provide a supporting statement explaining the medical necessity of the medication and why alternatives would have an adverse effect on your health. This process may require prior authorization, where your healthcare provider fills out a form explaining the need for the specific medication.
File an Appeal
If your request for an exception is denied, you have the option to file an appeal with your insurance company. This process varies depending on your insurer but typically involves submitting an application or a letter of appeal, often with the support of your doctor. They may need to provide additional documentation explaining the medical necessity of the medication. The appeal process can take some time, and you should receive a response within a specified timeframe, which may depend on the urgency of your situation.
Explore Alternative Options
While going through the exception and appeal process, it is worth discussing alternative treatment options with your doctor. There may be generic medications or similar drugs that can provide the same therapeutic benefits at a lower cost. Your doctor can guide you in exploring these alternatives and determining if they are suitable for your condition.
Patient Assistance Programs
If you are still facing challenges with coverage, patient assistance programs and manufacturer copay programs can provide financial support. These programs are often offered by drug manufacturers and charitable foundations to help individuals cover the cost of their medications. You can check the manufacturer's website or search for coupons and discounts for your specific medication. Additionally, some states and nonprofit organizations offer copay and premium assistance programs that can help reduce the cost of insurance and medication copays.
Remember that each insurance plan is different, and it is essential to understand your specific plan's coverage and appeal processes. Don't hesitate to reach out to your insurance provider and seek guidance from your healthcare team to navigate these steps effectively.
Understanding Loss Assessment: Unraveling the Intricacies of Shared Property Insurance Coverage
You may want to see also

If you are on your parents' insurance, they may be able to see your prescription records
However, you can take steps to protect your privacy. The Health Insurance Portability and Accountability Act (HIPAA) contains a privacy rule that allows patients to ask their insurer not to send an EOB form to their parents. Additionally, you can request that your insurer send EOBs to an alternate address or communicate with you at a different location. Some states, including California, Colorado, Washington, Oregon, and Maryland, have strengthened the health insurance confidentiality protections in HIPAA. Insurers in California, for example, must honor a member's request to withhold sensitive information from the policyholder.
If you are concerned about your parents seeing your prescription records, you can contact your insurance company to request that they send EOBs directly to you and change your contact information. You can also ask that they stipulate on your account that only you will be able to access your information unless you choose to release it to your parents. It is important to note that insurance companies are not obligated to honor requests to withhold information from the policyholder, and laws and company policies may vary depending on the state and insurer.
Additionally, if you are paying out of pocket for your prescriptions, your parents will not be able to see the details of your medication through insurance records.
Exploring Short-Term Insurance Options: Understanding the Array of Products Available
You may want to see also
Frequently asked questions
It depends on your insurance company. Some insurance companies will send out a list of medications purchased under the plan to the primary care holder. Other companies will not disclose this information unless it is requested by the primary care holder.
If you are concerned about your prescribed medication showing up on your insurance bill, you can contact your insurance company to ask about their specific policies. You can also pay for your medication out of pocket or go through your college health center or local health department.
You can call the number on the back of your insurance card and provide your insurance member ID, the name of the medication, and the prescribed dosage. You can also ask your pharmacist, use your insurance company's website or mobile app, or consult your plan's formulary (a list of the drugs that it covers).
If your insurance plan does not cover a medication you need, you can request an exception or a prior authorization. An exception can be made if you or your prescriber believe that none of the drugs covered by your insurance plan will work for your condition. A prior authorization may be required if your insurance plan needs confirmation that a particular drug is medically necessary for you.