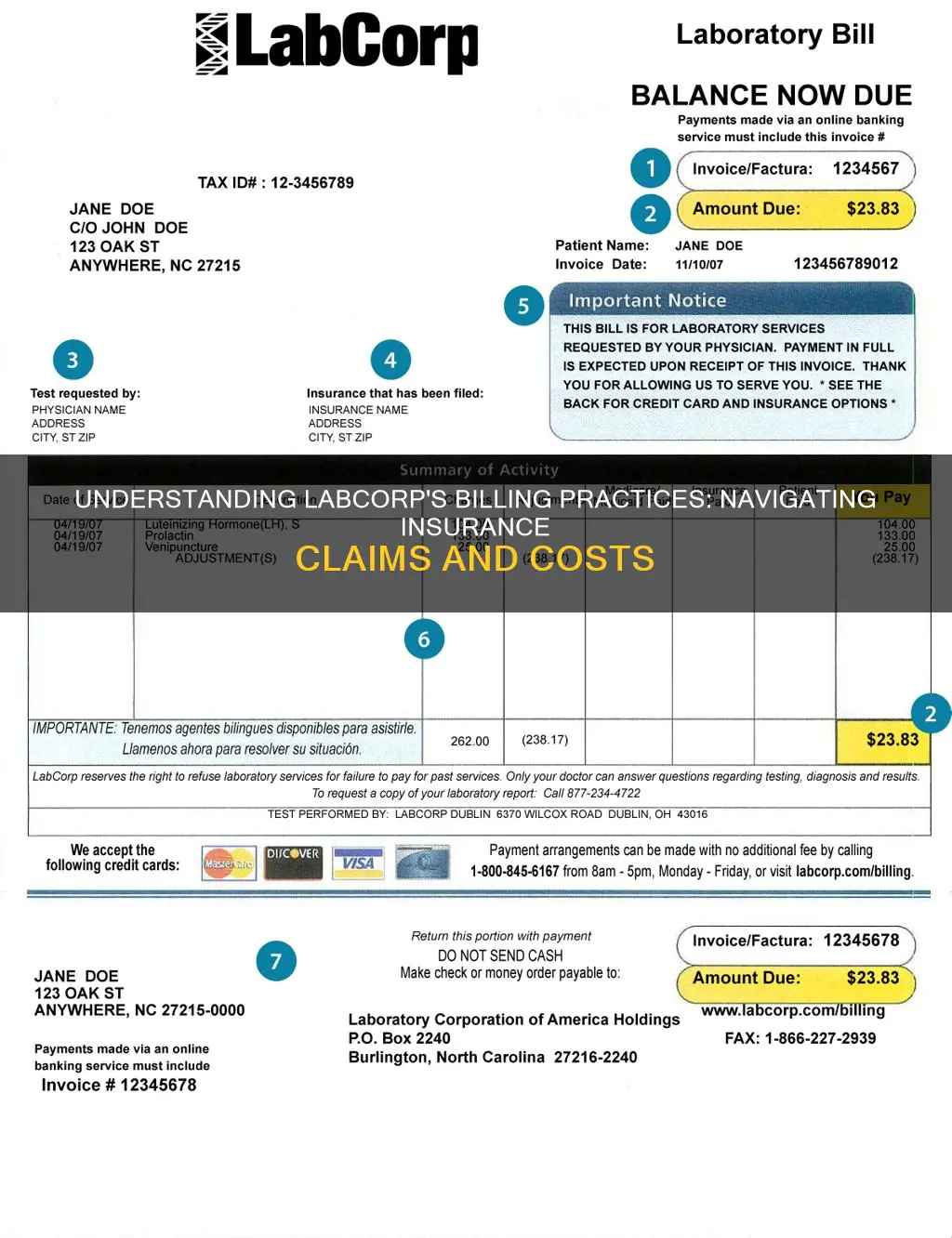
Labcorp offers a variety of payment options to patients, including billing insurance directly. Labcorp will bill Medicare and Medicaid, as well as many insurance companies and managed care plans. Patients are responsible for ensuring their insurance information is up to date and that Labcorp is a contracted laboratory for their insurance company. If a patient has more than one insurance plan, the primary insurer will process the claim first, and any remaining balance will be billed to the secondary insurer. If a balance remains after the secondary insurer has paid, Labcorp will send the patient a bill for the outstanding amount. Patients without insurance or whose insurance does not cover laboratory testing services will need to pay for tests before specimen collection services are performed.
| Characteristics | Values |
|---|---|
| Billing | Labcorp will bill your health insurance directly. |
| Insurance | Labcorp will bill Medicare and Medicaid. |
| Payment Methods | Website, toll-free telephone number, mail, in-person at patient service centers, cash, money orders, personal checks, and all major credit cards. |
| Payment Timing | Labcorp will send a bill approximately once a month until the balance is paid. |
| Insurance Response Time | Allow four to six weeks for the insurance company to process a claim. |
| Multiple Insurance Plans | Primary insurer processes the claim first, then the remaining balance is billed to the secondary insurer. |
| No Insurance | Patients must pay for tests before specimen collection services are performed. |
What You'll Learn

Payment methods
Labcorp offers a variety of payment options to its patients. If you receive a bill from Labcorp, you can make a payment through the following methods:
- Website: Visit the Bill Pay section, available 24 hours a day, 7 days a week.
- Toll-free telephone number: Call the automated voice response system at 800-845-6167, available 24 hours a day, 7 days a week.
- Mail: Send your payment to the address shown on your bill. Please remember to attach the stub from your bill when mailing in your payment. If paying by check, include your 8-digit invoice number on the check.
- Patient service centers: You may make payments in person at any of the Labcorp patient service centers.
Labcorp accepts cash, money orders, personal checks, and all major credit cards. For online payments, they also offer several convenient payment methods, including PayPal, Google Pay, and Apple Pay.
If you do not have insurance, you will have to pay for the tests performed by Labcorp before the specimen collection services are performed. An automated payment collection process is available at many of their patient service centers, as well as certain doctors' offices where a phlebotomist is on-site to perform specimen collection services for Labcorp.
Labcorp also offers programs to address the needs of patients with true financial hardship, including patient-specific payment plans, special payment plans for financial hardship, indigent requests from physicians/facilities, and the LabAccess Partnership program.
Understanding Secondary Insurance: Submitting Your Bills Efficiently
You may want to see also

Billing without insurance
If you do not have insurance, you will have to pay for the tests performed by Labcorp before specimen collection services are performed. An automated payment collection process is available at many of Labcorp's patient service centers, as well as certain doctors' offices where a phlebotomist is on-site to perform specimen collection services for Labcorp.
Labcorp offers a variety of payment options, including cash, money orders, personal checks, and all major credit cards. For online payments, Labcorp also offers several convenient payment methods, including PayPal, Google Pay, and Apple Pay.
Certain routine tests are available at discounted prices through the LabAccess Partnership program. To take advantage of this program, you must have your specimen collected at a Labcorp patient service center, and you must pay for your test in full at the time of service. The LabAccess Partnership (LAP) program is available for self-pay patients who are uninsured or whose health benefits exclude coverage for clinical laboratory testing services.
Under the law, patients who don’t have insurance or who are not using insurance may have the right to an estimate of the bill for medical items and services upon request or if they schedule an appointment at least 3 days in advance. Your estimate will include only the costs Labcorp will bill you for the lab services it is requested to perform. As a laboratory, Labcorp cannot reasonably predict what other medical services a patient may need and, therefore, cannot provide any estimated costs that may be charged by other unrelated health care providers or facilities, including any estimated charges by the health care provider who orders your laboratory test.
A Decade of Security: Unraveling the Benefits of 10-Year Level Term Insurance
You may want to see also

Billing with multiple insurance plans
Having multiple insurance plans can be beneficial in some cases, but it's important to understand how primary and secondary insurance works. Here's a guide to help you navigate billing when you have multiple insurance plans:
- Understanding Primary and Secondary Insurance: When you have multiple insurance plans, one plan is designated as the primary insurance, and the other becomes the secondary insurance. The primary insurance is responsible for paying first on any claims. The secondary insurance comes into play if the primary insurance is unable to cover the entire claim.
- Coordination of Benefits (COB): The Coordination of Benefits provision determines the order in which your insurance plans payout. It specifies which plan pays first, reduces the duplication of benefits, and increases the efficiency of claim processing. The COB rules are set by state and insurance providers and vary depending on the situation.
- Billing Process with Multiple Insurance Plans: When you receive healthcare services and have multiple insurance plans, the billing process works as follows:
- The healthcare provider files the claim with your primary health insurance company.
- The primary health insurer reviews the claim and pays according to your plan's benefits and coverage.
- The secondary health insurer then reviews the claim and pays for any remaining balance, based on their benefits and coverage.
- If there is still a balance remaining, the healthcare provider will bill you for the remaining amount.
- Labcorp Billing with Multiple Insurance Plans: If you have multiple insurance plans and receive services from Labcorp, they will bill your primary health insurance first. If there is a remaining balance, Labcorp will then bill your secondary insurance. If you receive a bill from Labcorp before receiving an Explanation of Benefits (EOB) from your secondary insurance, contact Labcorp Patient Billing to confirm that your secondary insurance information was received and a claim was filed.
- Pros and Cons of Multiple Insurance Plans: Having multiple insurance plans can offer certain advantages, such as increased coverage and reduced out-of-pocket costs. However, there are also potential drawbacks, including double premium and deductible payments, navigating multiple policies, and potential coverage overlap. It's important to carefully consider your specific situation before deciding to obtain a second insurance plan.
COBRA Coverage: Understanding Your Insurance Continuation Rights
You may want to see also

Billing with Medicare/Medicaid
Labcorp will file claims directly with Medicare, Medicaid, and many insurance companies and managed care plans. Before you have lab tests performed, you must ensure that your insurance information is up to date and that Labcorp is a contracted laboratory for your insurance company. You can contact your insurance company for this information.
Once your insurer has processed your claim, you will receive an Explanation of Benefits (EOB) from your insurer, informing you of the amount it will pay for your laboratory services. The EOB is not a bill, but it may indicate that a balance remains that is your responsibility. This balance may include your copayment, deductible, or other costs outlined in your terms of coverage. If you have a question about your EOB or your terms of coverage, contact your insurance company.
Your insurer will inform Labcorp about any balance you owe, and Labcorp will send you a bill for that amount.
If you are covered by more than one insurance plan, your primary insurer will process your claim first, and then any remaining balance will be billed to the secondary insurer. If a balance that is your responsibility remains after the secondary insurer has paid its portion of the claim, Labcorp will send you a bill for the balance due.
Updating Term Insurance: Changing Nominees and Ensuring Peace of Mind
You may want to see also

LabCorp's insurance carriers
LabCorp offers a variety of payment options to its patients, including billing insurance directly. Patients are advised to check with their insurance providers to see if LabCorp is a contracted laboratory provider.
LabCorp files claims directly with Medicare, Medicaid, and many insurance companies and managed care plans. The company provides a list of insurance carriers filed by LabCorp, which is available on its website. This list is not exhaustive and is subject to change.
To find a list of the insurance carriers filed by LabCorp, patients can visit the LabCorp website and select a state from the drop-down menu to view the corresponding PDF. The list includes insurance carriers from various states and regions, such as the District of Columbia, Wyoming, Wisconsin, Western Pennsylvania, West Virginia, and many more.
It is important for patients to verify and update their insurance information regularly, as well as to know which testing laboratories are in-network or participating providers for their benefit plan. This information can impact their level of coverage.
LabCorp also offers financial assistance programs for patients with true financial needs, including patient-specific payment plans, special payment plans for financial hardship, and the LabAccess Partnership program for uninsured or underinsured patients.
Infertility Clinics and the Insurance Billing Conundrum for Male Patients
You may want to see also
Frequently asked questions
If you do not have insurance, you will have to pay for the tests performed by Labcorp before specimen collection services are performed. An automated payment collection process is available at many of their patient service centers.
If your health care benefits do not cover clinical laboratory testing services, you will have to pay for the tests performed by Labcorp before specimen collection services are performed.
Labcorp relies on the ordering physician to submit the diagnosis code information at the time of the test order. Please contact your physician's office if your insurance company denied a claim due to the diagnosis code.