The time limit for insurance companies to back bill for prescription drugs varies depending on the state and the insurance provider. In general, insurance companies are allowed to back bill within a period of up to three years, although this can be as little as 90 days or even six months in some cases. In Florida, for example, the time limit is five years, whereas in New York it is two years. It is important to check with your state and insurance provider to understand the specific time limits that apply.
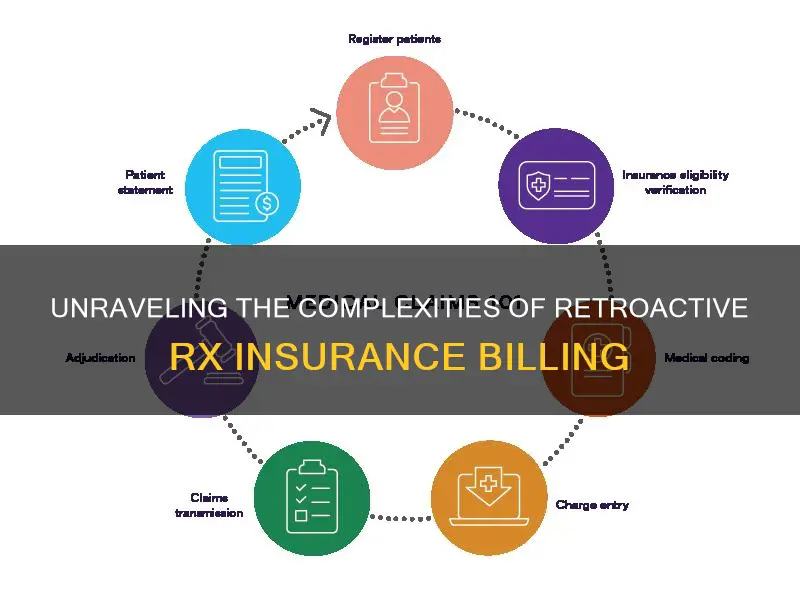
| Characteristics | Values |
|---|---|
| How far back can insurance cover medical bills? | Up to three years in the past depending on your coverage. |
| How long does a doctor's office have to send you a bill? | Up to six years from the date of the appointment to collect if there was a written agreement to pay. If there was no written agreement, the doctor’s office may have up to four years to collect. |
| Medical billing time limits | Varies by state. In Florida, it’s five years; New York is two years; Texas is no longer than the first day of the 11th month; California is 12 months. |
| Time limit for hospitals to bill | Normally within three to six years. |
| Time limit for insurance to cover past medical bills | Only up to the effective date of the policy. |
What You'll Learn
- Time limits for insurance to cover past medical bills vary from 90 days to three years
- Bills must be submitted within the deadline for them to be processed
- If a bill is out-of-network, it can be submitted for reimbursement
- If a policy has been cancelled, claims can still be filed for old bills
- If a claim is denied, an appeal can be made with additional details

Time limits for insurance to cover past medical bills vary from 90 days to three years
According to Adria Gross, founder of MedWise Insurance Advocacy, the time limits for medical billing vary from state to state. For example, in Florida, the time limit is five years, while in New York, it is two years. In Texas, the limit is the first day of the 11th month, and in California, it is 12 months.
It's important to note that these time limits refer to how long the medical provider has to submit a claim to the payer, which can be the patient or their insurance company. The patient is still required to pay the medical bills they incur, either directly or through their insurance.
Additionally, the time limit for insurance coverage of past medical bills also depends on the effective date of the policy. The coverage typically begins on the effective date, and any medical services provided before this date will not be covered. In some cases, employers may offer a grace period to enroll in health insurance, and the coverage can be backdated to the date the employee was initially eligible.
To ensure timely reimbursement, it is recommended to file insurance claims as soon as possible and to check with the insurance provider about specific time limits and deadlines, especially when switching plans or insurance providers.
United Short-Term Insurance: Understanding the HMO-PPO Hybrid Model
You may want to see also

Bills must be submitted within the deadline for them to be processed
It is imperative to submit insurance claims on time to ensure that they are processed and paid out. The deadline for submitting a claim varies depending on the insurance provider and the state. In some states, the deadline is as little as 90 days, while others allow up to three years for claims to be submitted. It is important to check with your specific insurance provider to find out their deadline for submitting claims.
The consequences of missing the deadline can vary. In some cases, the insurance provider may still pay the claim even if it is submitted after the deadline. However, this is not guaranteed, and the longer you wait to submit the claim, the less likely it is that the provider will pay it. If the insurance company denies the claim due to untimely submission, you may be responsible for the full amount of the bill.
To avoid missing the deadline, it is recommended to submit claims as soon as possible after receiving the medical service. It is also important to keep track of your medical bills and confirm that they have been paid by your insurance company. If you notice any discrepancies or unpaid bills, contact your insurance provider immediately to resolve the issue.
Additionally, it is worth noting that the deadline for submitting a claim may differ from the standard repayment time for a medical bill. The standard repayment time is typically 30 days after receiving the bill. However, this may vary depending on the provider or hospital, so it is essential to check with them directly to confirm the allowable payment timeframe.
Billing Blue Cross Blue Shield Insurance: A Step-by-Step Guide
You may want to see also

If a bill is out-of-network, it can be submitted for reimbursement
If your plan includes out-of-network coverage, your insurance company might pay part of the bill. However, you will be responsible for whatever isn't covered by your insurance, which will be the full amount if your plan only covers in-network care or if you haven't yet met your out-of-network cost-sharing.
In the US, the No Surprises Act, which came into effect in 2022, provides some protection for consumers against surprise medical bills. This includes emergency services and non-emergency services provided by out-of-network providers at in-network facilities. Under this law, health plans must cover surprise bills at in-network rates, and balance billing is prohibited.
It's worth noting that the rules and regulations regarding medical billing time limits vary by state. It's recommended to check with your state to see what the limit is, as medical providers are often allowed several years to send you a bill.
To submit an out-of-network bill for reimbursement, you will need to follow the process outlined by your insurance provider. This may involve submitting the bill along with any relevant documentation to support your claim. It's important to review the terms and conditions of your insurance policy to understand what is covered and what the time limits are for submitting claims.
The Safety Net: Understanding the Ins and Outs of Insuring Treasury Bills
You may want to see also

If a policy has been cancelled, claims can still be filed for old bills
If your insurance policy has been cancelled, you may still be able to file claims for old bills. However, the process may be more complex and there are a few things to keep in mind. Firstly, you should contact your insurance provider as soon as possible to understand your options. In some cases, you may be able to reinstate your policy, especially if the cancellation was due to a missed payment. There is usually a grace period, typically between 10 to 20 days, during which you can make the payment and reinstate your coverage without any lapse. If the grace period has passed, your insurance company may still reinstate your policy, but there is no guarantee.
If your policy cannot be reinstated, you will need to purchase a new insurance policy. A lapse in coverage may result in higher rates and some insurers may not offer you coverage, considering you a high-risk driver. In this case, you may need to turn to companies that specialise in insuring high-risk drivers. It is worth getting multiple quotes to find the best rate. Additionally, you can join your state's assigned risk pool, which is a group of insurers that accept high-risk drivers.
It is important to note that if your policy was cancelled due to non-payment, you may still owe money to your previous insurance company. They may pass any overdue debts to a collection agency, which can negatively impact your credit score. Therefore, it is crucial to communicate with your insurance company and make arrangements to resolve any outstanding payments.
Regarding filing claims for old bills, it is important to review the specific terms of your policy. In general, you can cancel an auto insurance claim that you have filed, even after receiving a reimbursement check, as long as you have not cashed it. However, if the accident was your fault and someone has filed a claim against you, you cannot cancel that claim. Additionally, if you have already cashed the reimbursement check, you can contact your insurance company to inquire about cancelling the claim if you return the funds.
Understanding the Implications of Short-Term Insurance Overlap
You may want to see also

If a claim is denied, an appeal can be made with additional details
If your prescription claim is denied, you can make an appeal by requesting your insurance company to reconsider its decision. The appeal process usually has three levels.
First-Level Appeal — You or your doctor can contact your insurance company and request them to reconsider the denial. Your doctor may also request to speak with the medical reviewer of the insurance plan as part of a "peer-to-peer insurance review" to challenge the decision. The purpose of the first appeal is to prove that your service meets the insurance guidelines and that it was incorrectly rejected.
Second-Level Appeal — In this step, the appeal is reviewed by a medical director at your insurance company who was not involved in the claim decision. The goal of this appeal is to prove that the request should be accepted within the coverage guidelines.
Independent External Review — In an external review, an independent reviewer from the insurance company and a doctor with the same specialty as your doctor assess your appeal to determine if they will approve or deny coverage. People often turn to an external review if an internal appeal is not possible or is unsuccessful.
Before starting the appeal process, you should find out why your claim was denied. Your claim may be denied due to an error in the claim documents, your plan not covering the service you're claiming, the service being deemed not medically necessary, your plan not covering the out-of-network provider, or you having reached the coverage maximum of your plan.
You can start the appeal process by calling your insurance provider and asking for more details about the denial and reviewing your appeal options. You should also call your doctor's office to check if they left out important information on the claim form or used the wrong code when submitting the claim. If this is the case, you can ask your doctor to resubmit the claim and correct the error. If the claim was denied for another reason, let your doctor know that you're appealing, and ask them to write a letter explaining that the service was medically necessary or to provide other supporting documents.
To submit an appeal, you will need to fill out the required forms and write an appeal letter. The letter should include:
- What service was denied and why.
- Why your claim should be paid, with supporting evidence from your plan policy documents.
- An overview of your health condition and details about why the service is medically necessary.
- Supporting evidence, such as medical records or a letter from your doctor.
Your insurance provider is required to make a decision quickly. If you're appealing coverage for a treatment you have not received, they must make a decision within 30 days. If you've already received treatment, they must reply within 60 days. If you're appealing a claim denial for urgent care, your insurance company must decide within 72 hours.
Understanding Term Insurance: A Guide to Unraveling the Basics
You may want to see also
Frequently asked questions
There is no set time period for how far back insurance can cover your medical bills, but it is recommended to file claims as soon as possible. The time period varies depending on the state and the insurance provider. Some providers will cover up to three years in the past, while others have a limit of ninety days.
Yes, the date of service is important. The service date should fall within the plan year for the claim to be passed, otherwise, the filed claim will be denied.
No, your new insurance will not cover an old medical bill with a service date before the coverage effective date.
If your insurance policy has been terminated, any medical bills incurred after the termination date will not be paid.
If your claim is denied, you can make an appeal claim. You can provide additional details or circumstances that might support your case.