Hepatitis C is a bloodborne virus that affects the liver and can cause acute and chronic hepatitis. It is transmitted through contact with infected blood, commonly through unsafe injection practices, unsafe healthcare, and the transfusion of unscreened blood. While there is currently no effective vaccine, the disease can be cured with direct-acting antiviral medications, which have a success rate of over 95%.
In the United States, it is estimated that there are around 2.4 million people infected with Hepatitis C, with a prevalence of 0.93%. However, approximately half of those infected are unaware of their diagnosis. The virus disproportionately affects certain groups, such as people who inject drugs, incarcerated people, people in rural areas, and those without access to preventive healthcare.
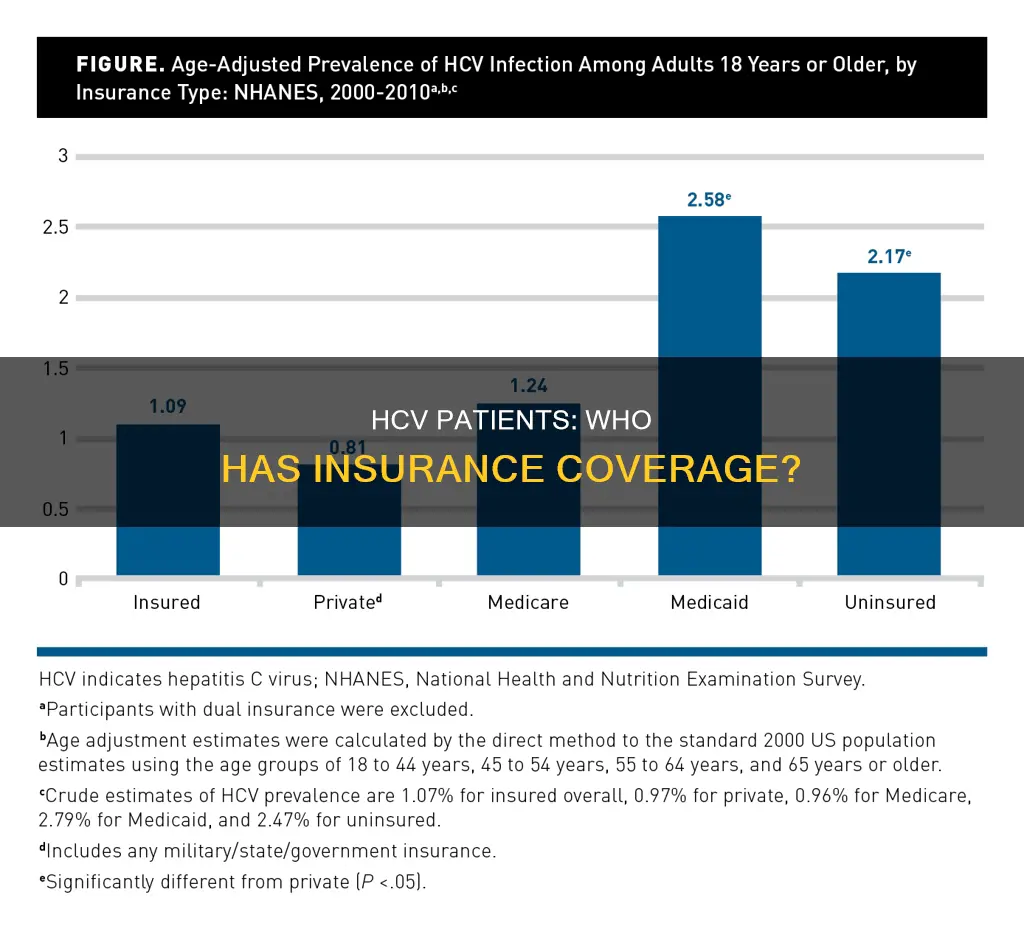
Insurance coverage plays a significant role in the treatment and management of Hepatitis C. Studies have shown that insurance coverage for Hepatitis C patients is inadequate globally, with many patients lacking insurance programs. This poses a challenge for ensuring effective treatment, as the high costs of medications create barriers to access. In the United States, the Medicaid population has a significantly higher prevalence and mortality rate from Hepatitis C compared to patients with private insurance. This highlights the need for policymakers to prioritize funding and support for Medicaid programs to address the disease.
The lack of insurance coverage among Hepatitis C patients can lead to challenges in diagnosis, treatment, and linkage to care. It is crucial to bridge the gap for uninsured patients to improve their access to diagnosis and treatment, especially among high-risk groups.
| Characteristics | Values |
|---|---|
| Prevalence of HCV | 0.93% of the US population (approximately 2.4 million people) |
| Undiagnosed HCV | 45-85% of HCV-infected individuals |
| HCV-related complications | Diabetes (15% of patients), depression (25% of patients) |
| HCV-related costs | $280 for an uncomplicated hepatitis to $139,070 for a liver transplantation |
| HCV-infected individuals with insurance | More likely to be diagnosed and treated |
| HCV-infected individuals without insurance | Less likely to be diagnosed and treated |
What You'll Learn
- HCV-infected patients with Medicaid have a higher risk of all-cause mortality than those with private insurance
- HCV-infected patients are more likely to be uninsured or covered by Medicaid
- HCV-infected patients with insurance are more likely to be diagnosed than those without insurance
- HCV-infected patients with government insurance are more likely to be diagnosed than those without insurance
- HCV-infected patients with private insurance are more likely to be diagnosed than those without insurance

HCV-infected patients with Medicaid have a higher risk of all-cause mortality than those with private insurance
A study published in the American Journal of Managed Care in 2019 analysed data from the National Health and Nutrition Examination Survey from 2000 to 2010. Among the 19,452 eligible participants, 311 (1.4%) were HCV-positive. The study found that HCV-positive patients were more likely to be covered by Medicaid or be uninsured compared to HCV-negative patients. After adjusting for confounders, HCV-positive patients with Medicaid coverage had an increased risk of mortality compared to those with private insurance (hazard ratio [HR] 6.31, 95% CI 1.22-29.94) and uninsured individuals (HR 8.83, 95% CI 1.56-49.99).
The study highlights the need for policymakers to prioritise funding and support for Medicaid programs to address the high burden of HCV infection and adverse prognosis among this population. Restricted access to HCV medication among Medicaid patients remains an issue, and further research is needed to assess the impact of Medicaid expansion and changes in payer coverage for HCV treatment.
Another study presented at Digestive Disease Week in 2018 also found that HCV-positive patients with Medicaid had a higher risk of mortality compared to those with private insurance. The study analysed data from the NHANES database from 2000 to 2010 and found that HCV-positive patients with Medicaid had a higher risk of mortality (HR 9.64, 95% CI 1.66-55.97). The study concluded that having public insurance, especially Medicaid, increases the risk of mortality in HCV-infected patients.
These findings emphasise the importance of providing adequate coverage and access to care for HCV-infected patients with public insurance, particularly those on Medicaid.
Hit and Run: Insurance and Legal Consequences
You may want to see also

HCV-infected patients are more likely to be uninsured or covered by Medicaid
Several studies have found that HCV patients without insurance or with Medicaid coverage have a higher risk of mortality compared to those with private insurance. In one study, the risk of death for HCV-positive patients with Medicaid was almost 10 times higher than for those with private insurance. Another study found that HCV patients with public insurance or no insurance had higher mortality rates than those with private insurance. The increased risk of death among HCV patients with Medicaid was attributed to a higher prevalence of comorbidities such as diabetes, congestive heart failure, and stroke.
The high cost of HCV treatment is a significant barrier for many patients, especially those without insurance or with Medicaid. Direct-acting antiviral agents (DAAs) have cure rates above 96%, but their high efficacy comes with substantial budgetary implications. Medicaid programs, in particular, struggle to cover the cost of these treatments, often imposing substantial access restrictions. Prior authorization requirements for DAAs vary by state, and the paperwork burden falls on already stretched physician offices, leading to delays in treatment.
Challenges in diagnosing HCV also contribute to the higher uninsured rate among HCV patients. Early detection and treatment can prevent serious liver damage and improve long-term health outcomes. However, many people with new HCV infections are asymptomatic, and the infection often remains undetected until symptoms develop decades later when serious liver damage has occurred. Testing and diagnosis of HCV involve multiple steps, and innovative new tests are in the pipeline to enable simpler and faster diagnosis.
The association between HCV infection and insurance status has important implications for health outcomes. HCV-infected patients without insurance or with Medicaid coverage face barriers to accessing timely and appropriate care, leading to poorer health outcomes and increased mortality rates. Policy interventions are needed to improve access to HCV treatment and support Medicaid programs in covering the high costs.
Insurance Switch: When to Change?
You may want to see also

HCV-infected patients with insurance are more likely to be diagnosed than those without insurance
In the United States, the affordability of healthcare is largely dependent on insurance type. Some types of insurance cover nearly all the upfront costs of medications, while others require individuals to pay large sums of money out of pocket. This can create potential barriers to accessing beneficial treatment. This is especially relevant for new anti-HCV regimens that are highly effective but also carry a substantial financial burden. As a result, some payers, particularly state Medicaid programs, have placed substantial access restrictions on these treatments.
A study by the National Health and Nutrition Examination Survey (NHANES) found that among HCV-infected individuals, those with Medicaid coverage had an increased risk of mortality compared to those with private insurance. This highlights the importance of insurance coverage in providing access to timely diagnosis and treatment, which can improve health outcomes for patients with HCV.
Another study found that HCV-infected patients with private insurance were more likely to receive treatment compared to those with public aid or no insurance. This suggests that insurance coverage plays a significant role in facilitating access to treatment and improving health outcomes for HCV-infected individuals.
The high cost of HCV treatment remains a challenge, and it is important to address the financial burden faced by patients, especially those with Medicaid or no insurance. Negotiations between healthcare decision-makers and insurance managers are crucial to ensuring that all patients have access to the necessary treatment and improving health outcomes, especially for those at higher risk of developing cirrhosis and liver cancer.
Maximizing Insurance Billing: Strategies for Savvy Contractors
You may want to see also

HCV-infected patients with government insurance are more likely to be diagnosed than those without insurance
Hepatitis C is a global public health challenge that imposes a significant economic burden on countries worldwide. The disease is caused by the hepatitis C virus (HCV), which affects the liver and can lead to acute and chronic hepatitis. While effective treatments are available, insurance coverage for HCV patients is often inadequate, and the high cost of treatment creates barriers to access.
In the United States, the prevalence of HCV infection between 2013 and 2016 was estimated at 0.93%, translating to approximately 2.4 million infected individuals. However, it is believed that about half of those infected are unaware of their diagnosis. The lack of diagnosis is particularly prevalent among certain groups, such as people who inject drugs, incarcerated individuals, people in rural areas, and those without routine access to healthcare.
Insurance status plays a significant role in the diagnosis and treatment of HCV. A study in California found that HCV-infected individuals with government insurance were more likely to be diagnosed than those without insurance. The relative risk of HCV diagnosis was significantly higher for those with government insurance compared to the uninsured (RRR = 10.61) and those with private insurance compared to the uninsured (RRR = 6.79). This disparity highlights the critical need for increased viral load testing and linkage to care for uninsured individuals.
The high cost of HCV treatment, which can reach up to $100,000 per course, poses a significant challenge. Direct-acting antiviral medications (DAAs) have proven highly effective, with cure rates exceeding 95%. However, the expense of these drugs creates barriers for many patients, particularly those without insurance.
To address these challenges, efforts should focus on reducing treatment costs and improving patient support. Insurance providers play a crucial role in this regard, as they can help offset financial burdens and ensure continuity of care. Moreover, the integration of various insurance programs can lead to greater value and clinical safety. Negotiations between healthcare decision-makers and insurance managers are essential to bridge the gap and ensure access to treatment for all, regardless of insurance status.
Medi-Cal: ACA Insurance or Not?
You may want to see also

HCV-infected patients with private insurance are more likely to be diagnosed than those without insurance
Better Access to Healthcare Services
HCV-infected patients with private insurance often have better access to healthcare services, including regular check-ups, screenings, and diagnostic tests. This is because they can afford the high costs associated with medical care and are more likely to have a regular source of care. Having a regular source of care increases the chances of receiving appropriate care and being diagnosed.
Higher Rates of Health Insurance Coverage
HCV-infected patients with private insurance are more likely to have health insurance coverage, which provides financial protection against the high costs of medical care. This means that they are more likely to seek medical attention and get diagnosed if they experience any symptoms or health issues related to HCV infection.
More Effective Treatment Options
HCV-infected patients with private insurance may have access to more effective treatment options, such as direct-acting antivirals (DAAs), which have high cure rates and fewer side effects compared to traditional interferon-based regimens. The availability of these treatments can increase the likelihood of HCV-infected patients seeking medical care and getting diagnosed.
In conclusion, HCV-infected patients with private insurance are more likely to be diagnosed than those without insurance due to better access to healthcare services, higher rates of health insurance coverage, and more effective treatment options. These factors contribute to increased rates of diagnosis and better health outcomes for HCV-infected patients with private insurance.
Marketplace Insurance: Public Charge Rule Change Impact
You may want to see also
Frequently asked questions
It is estimated that around 30% of people with HCV do not have insurance.
Insurance status can have a significant impact on HCV treatment. Studies have shown that patients with insurance are more likely to be diagnosed and treated for HCV compared to those without insurance. This is mainly due to the high cost of HCV medications, which can be a barrier for uninsured patients.
The high cost of HCV medications, prior insurance authorization, and lack of health insurance are some of the main barriers to HCV treatment for uninsured patients. These factors can prevent patients from accessing treatment and lead to disruptions in care.
Insurance status can also affect HCV diagnosis and linkage to care. Uninsured patients may have lower odds of being diagnosed with HCV and linked to appropriate care services. This can result in undetected infections and delayed treatment, increasing the risk of liver-related complications.