An insurance verifier is a healthcare professional who ensures that patients' insurance policies cover their required medical procedures. They are responsible for reviewing and verifying patient insurance information, billing, and patient claims. This involves contacting insurance companies, sending documentation, and billing them for procedures. To become an insurance verifier, you typically need a high school diploma and some relevant work experience, although a bachelor's degree in a relevant field and additional certifications can increase your competitiveness as a candidate.
| Characteristics | Values |
|---|---|
| Education | High school diploma, associate's degree in medical administration or a related health field, or bachelor's degree in business, finance, or healthcare administration |
| Work Experience | 2-4 years in roles such as customer service or data entry, or none to less than 1 month of relevant work experience |
| Training | On-site or on-the-job training for 1-3 months |
| Certifications | Health Insurance Portability and Accountability Act (HIPAA) Certification, Certified Billing and Coding Specialist (CBCS), Certified Medical Administrative Assistant (CMAA) |
| Skills | Strong communication, organizational, and data entry skills; attention to detail; knowledge of medical terminology, insurance, and hospital billing policies and procedures |
| Duties and Responsibilities | Verify insurance coverage for new and existing patients, update patient information, obtain pre-authorization for services, explain financial responsibilities to patients, answer billing and insurance questions |
What You'll Learn
- Education: A high school diploma, associate's or bachelor's degree in a relevant field such as business, finance, or healthcare administration
- Experience: 2-4 years of relevant work experience in roles like customer service or data entry
- Skills: Strong communication, organisational, and data entry skills, along with attention to detail
- Training: On-site or on-the-job training for 1-3 months to learn specific processes and systems
- Certifications: Gain additional certifications like Certified Billing and Coding Specialist (CBCS) or Certified Medical Administrative Assistant (CMAA) to stand out to employers

Education: A high school diploma, associate's or bachelor's degree in a relevant field such as business, finance, or healthcare administration
A high school diploma is the minimum level of education required to become an insurance verifier or specialist. However, some employers may prefer candidates with an associate's or bachelor's degree in a relevant field such as business, finance, or healthcare administration. Obtaining a degree in these fields can provide a strong foundation of knowledge and skills for a career in insurance verification.
An associate's degree in medical administration or a related health field can be beneficial for understanding the basics of patient privacy law, medical billing, and hospital administrative duties. This type of degree can also prepare individuals for the specific tasks and responsibilities of an insurance verifier, such as verifying patient information, billing, and conducting claims examinations.
On the other hand, a bachelor's degree in a relevant field can enhance one's skills and knowledge in insurance verification. Pursuing a degree in business, finance, or healthcare administration can equip individuals with strong communication, organisational, and problem-solving skills, which are highly valued in the insurance verification field.
In addition to educational qualifications, gaining relevant work experience is also crucial for becoming an insurance verifier. This can include working in customer service or data entry roles to develop communication, organisation, and attention to detail skills. On-the-job training is often provided by employers, allowing individuals to learn the specific processes and systems used in insurance verification.
Flexeril: Insurance Companies Denying Seniors
You may want to see also

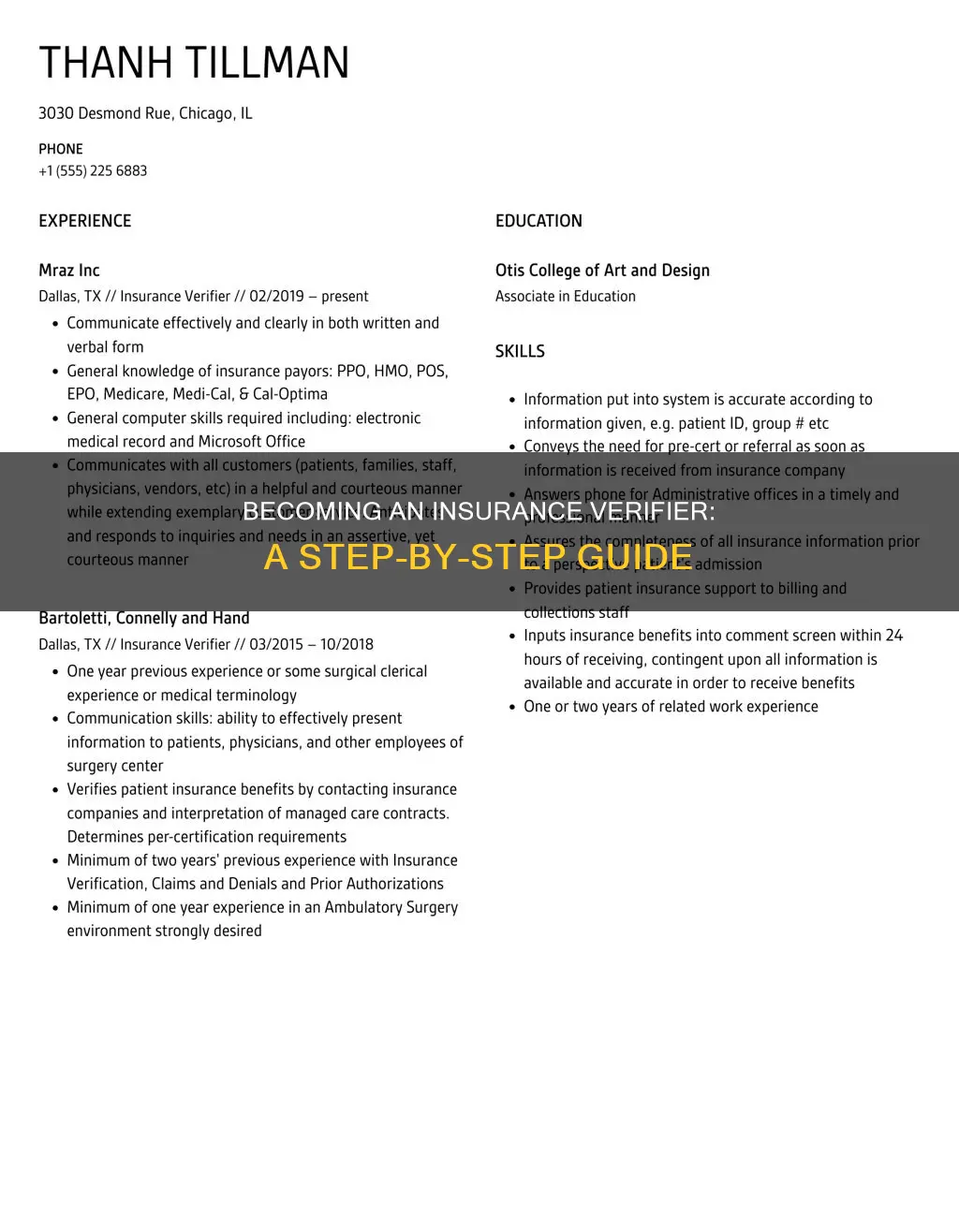
Experience: 2-4 years of relevant work experience in roles like customer service or data entry
To become an insurance verifier, you'll typically need 2-4 years of relevant work experience in roles such as customer service or data entry. This will help you develop essential skills in communication, organisation, and attention to detail.
In a customer service role, you will hone your communication skills by interacting with customers and providing support and assistance. You will also learn to manage customer expectations and resolve any issues or concerns they may have. These skills will be invaluable as an insurance verifier, as you will need to communicate effectively with both insurance companies and patients.
Data entry roles, on the other hand, will help you develop your organisational and attention to detail skills. Accurate and efficient data entry is crucial in medical and insurance records, as errors can have significant consequences. By gaining experience in data entry, you will become proficient in managing large amounts of information and ensuring its accuracy and confidentiality.
During these initial years, you may also consider pursuing an associate's degree in medical administration or a related health field. This is not always necessary, as some insurance verifier positions only require a high school diploma. However, an associate's degree can provide you with valuable knowledge in patient privacy law, medical billing, and hospital administrative duties.
Additionally, you may want to obtain voluntary certifications, such as the Health Insurance Portability and Accountability Act (HIPAA) Certification, to boost your credentials and increase your competitiveness in the job market.
Healthcare Insurance: Who's Covered?
You may want to see also

Skills: Strong communication, organisational, and data entry skills, along with attention to detail
Strong communication skills are essential for insurance verifiers, as they must be able to clearly convey information to both insurance companies and patients. They need to be able to explain complex insurance concepts in a way that patients can understand, such as coverage amounts and why certain procedures are or aren't covered. Verifiers also need to be confident communicators when negotiating payment arrangements and liaising between patients and providers. Strong communication skills also encompass listening carefully and responding effectively to patients' queries and concerns. Bilingual communication skills, particularly English/Spanish, are highly desirable in this field.
Organisational skills are another key requirement for insurance verifiers. They need to be able to manage and maintain accurate patient records, ensuring all information is up-to-date and easily accessible. This includes verifying and updating patient insurance information, as well as coordinating payment arrangements and entering patient data into computer systems. Organisational skills are also important for multitasking and managing the high volume of phone calls and paperwork associated with the role.
Data entry skills are vital for insurance verifiers, as they are responsible for accurately entering and updating patient information in computer systems. This includes entering patient demographic information, insurance details, and benefit coverage findings. Attention to detail is crucial for this aspect of the role, as even small errors can lead to claim denials and disruptions in patient care.
Elective Insurance Change: Know the Law
You may want to see also

Training: On-site or on-the-job training for 1-3 months to learn specific processes and systems
On-the-job training is a crucial aspect of becoming an insurance verifier. This phase typically occurs in the third or fourth year of your journey and lasts for around 1-3 months. During this time, you'll dive deep into the specific processes and systems used in insurance verification, which will vary depending on the employer and their chosen systems.
While gaining relevant work experience in customer service or data entry roles, you will also be preparing for this on-site training. This initial work experience will help you develop the fundamental skills required for insurance verification, including communication, organisation, and attention to detail.
The on-site training will build upon this foundation, teaching you the specific skills and techniques required for insurance verification. This includes learning how to review and verify insurance documents, handle patient registration, negotiate payment arrangements, and perform data entry of complex information. You will also become proficient in coordinating benefits, investigating and completing prior authorisation processes, and ensuring patient account information is accurate and up-to-date.
This training is essential to ensure you can competently and confidently perform the duties of an insurance verifier, which include verifying insurance coverage, processing payments, and providing excellent customer assistance.
Remember, each employer will have unique qualifications and requirements, so be sure to research the specific on-site training programs offered by the companies you're interested in working for.
Navigating Insurance Policies: Understanding When Change is Necessary
You may want to see also

Certifications: Gain additional certifications like Certified Billing and Coding Specialist (CBCS) or Certified Medical Administrative Assistant (CMAA) to stand out to employers
Gaining additional certifications is a great way to stand out to employers when applying for insurance verifier roles. Two certifications that are particularly useful are the Certified Billing and Coding Specialist (CBCS) and Certified Medical Administrative Assistant (CMAA) certifications.
The CBCS certification is a great way to demonstrate competence in billing and coding, which are essential skills for insurance verifiers. The CBCS exam covers both billing and coding activities, giving you a strong foundation in these areas. Many employers require or encourage certification for billing and coding specialists, so having this certification can make you a more attractive candidate.
The CMAA certification, on the other hand, focuses on providing administrative support in a medical setting. This certification will prepare you for a variety of administrative duties, as well as direct patient contact in clinical settings. CMAA certification can be especially useful if you're interested in working in healthcare offices or other medical administrative roles.
Both the CBCS and CMAA certifications are recognised by employers as valuable qualifications. They demonstrate your knowledge, skills, and commitment to the field. These certifications can help you access better career opportunities and maximise your earning potential.
To be eligible for the CBCS and CMAA exams, you typically need a high school diploma or equivalent, and some relevant work experience is often preferred. The exams may be taken online or in person, and there are various study materials available to help you prepare.
Tricare: Government-Sponsored Insurance
You may want to see also
Frequently asked questions
The minimum qualification to become an insurance verifier is a high school diploma. However, some employers may require an associate's degree in medical administration or a related health field. Gaining work experience in customer service or data entry roles can also be beneficial.
Insurance verifiers need strong communication, organisational, and data entry skills. They must also be detail-oriented, able to multitask, and have knowledge of different insurance policies and coverage types.
Insurance verifiers review and verify patient insurance information, ensure treatments are covered by insurance policies, and communicate with patients and insurance providers about benefits, coverage, and authorisations. They also handle billing processes and patient claims.
It typically takes 2-4 years to become an insurance verifier, including gaining relevant work experience and completing on-the-job training.