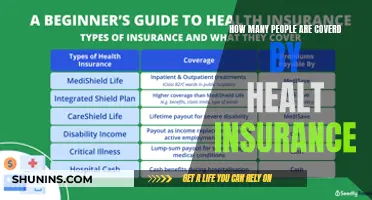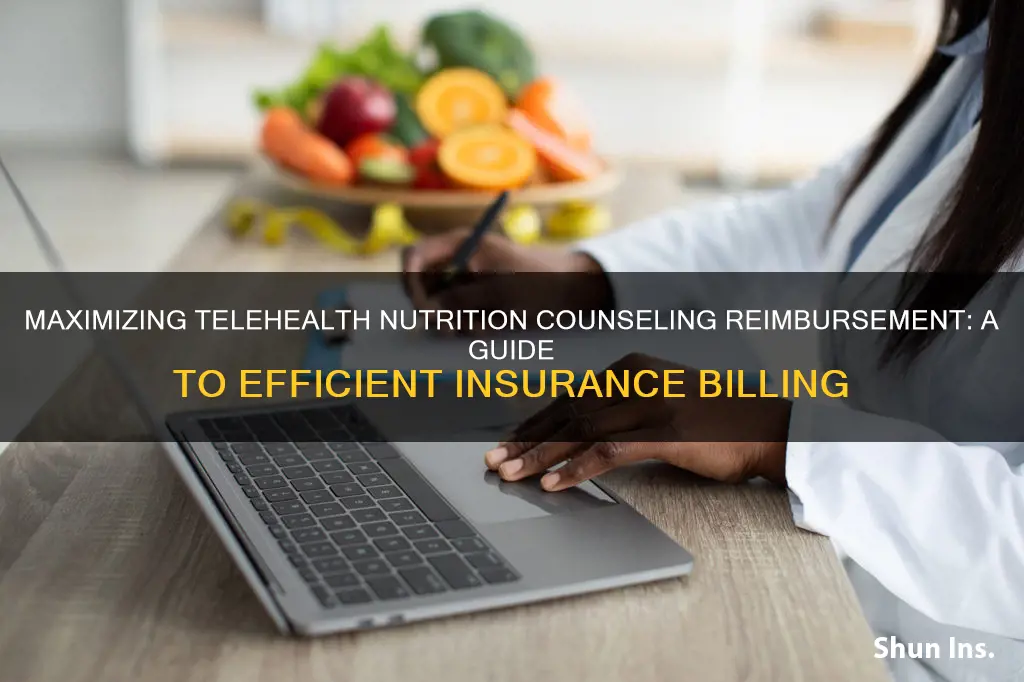
Telehealth nutrition counselling is a rapidly growing sector of the virtual healthcare industry. It is a natural extension of health and wellness services, as most counselling and coaching services can be completed virtually, with no physical contact. The benefits of offering virtual nutrition services extend to both providers and clients. Nutrition professionals are able to reach more clients, have more frequent check-ins, and provide ongoing and real-time support.
If you are a dietitian or nutrition professional, you may be wondering how to bill insurance for telehealth nutrition counselling services. This can be a complex process, as there is no uniform approach to telehealth reimbursement, regulation, and policy. The process will depend on the state and insurance provider, and whether you are an in-network or out-of-network provider.
1. Verify Insurance Coverage: Contact the insurance company to check if telehealth visits are covered for specific CPT (Current Procedural Terminology) codes, such as 97802 for initial consultations and 97803 for follow-up consultations.
2. Understand In-Network and Out-of-Network Coverage: If you are an in-network provider, you will charge the client for any deductible, co-pay, or co-insurance not covered by their insurance. If you are out-of-network, you can still bill the insurance, but the client will need to pay the full cost of the appointment upfront and will be reimbursed by the insurance company directly.
3. Obtain Informed Consent: Obtain informed consent from clients for virtual counselling services, outlining the benefits and risks associated with participating in telehealth services.
4. Use a HIPAA-Compliant Platform: Ensure that you use a secure, HIPAA-compliant telehealth platform for your virtual sessions, as phone, Skype, and Facetime are not considered HIPAA-compliant.
5. Verify Coverage with the Client's Insurance Provider: Call the insurance provider to verbally confirm telehealth coverage and clarify their definition of telehealth (video-chat only or including phone calls).
6. Check Professional Liability Insurance Coverage: Make sure your professional liability insurance covers telehealth services.
7. Submit CMS 1500 Claims: If the client's insurance covers virtual nutrition services, you will need to adjust the Place of Service (POS) code on the CMS 1500 claim to 02 for the telehealth nutrition session.
8. Provide a Superbill: If the client self-pays, provide them with a Superbill, a detailed receipt of services that includes all the information the insurance company needs to process a healthcare claim.
9. Obtain Payment: Put in place a financial agreement policy, clearly indicating the client's responsibility for payment if insurance does not approve their claim. Collect copays at the time of service, unless specified otherwise.
Remember, this is a general guide, and the specific steps may vary depending on your location and the insurance providers you work with. It is important to familiarize yourself with the legal considerations and requirements for telehealth services in your state.
| Characteristics | Values |
|---|---|
| CPT codes for nutrition services | 97802, 97803, 97804, 98966, 98967, 98968, 99402, 99403, 99404, 99411, 99412, 99443, S9470 |
| HCPCS codes for nutrition services | G0270, G0271, G0108, G0109, G0447 |
| CPT codes for diabetes self-management training | G0108, G0109 |
| ICD-10 code for preventative nutrition counselling | Z71.3 |
| ICD-10 codes for medical nutrition therapy for a specific disease or condition | E11, R73.09, E66.9, E78.5, K58.0/K58.9, I10, K90.0, Z91.01 |
| Telehealth CPT codes | 99441, 99442, 99443, G0438, G0439 |
| Telehealth HCPCS codes | G0396, G0397, G0442, G0443, G0444, G0445, G0446, G0447 |
| Telehealth POS code | 02 |
| Telehealth platform requirements | HIPAA-compliant; may need to be specified by insurance company |
| Insurance types | Private, public, Medicare, Medicaid |
| Private insurance companies | UnitedHealthcare, Cigna, Aetna, Anthem Blue Cross Blue Shield |
| Public insurance companies | Medicare, Medicaid |
What You'll Learn

Understanding insurance reimbursement
Credentialing and Contracting
To become an in-network provider, you will need to go through the credentialing and contracting processes. Credentialing involves becoming "credentialed" with the carriers of your choice, for which you will need an Employer Identification Number, a license (if required in your state), a National Provider Identifier (NPI), and liability insurance. Contracting is the process of becoming an in-network provider with insurance companies and establishing the policies and guidelines for filing claims for plan members.
Billing Codes
When billing insurance companies, you will indicate a billing code on your CMS1500 claim for each client encounter. The billing code will correspond to the service provided, and the insurance company will have a designated reimbursement rate for that code. It is important to be aware of the different billing codes and to confirm with the insurance company which codes they cover.
Telehealth Services
Telehealth services can be covered by insurance, but it is important to note that there is variance in how insurance companies define and reimburse for these services. It is recommended to call the insurance provider in advance to verbally confirm telehealth coverage and clarify how the insurance carrier classifies telehealth.
Reimbursement Rates
Each insurance company will have a different reimbursement rate, and it is important to research what is considered a competitive rate for your geographic location. The reimbursement rate may be set as a percentage of the Medicare fee schedule or as a set dollar amount per time. It may be possible to negotiate a higher reimbursement level from the carrier.
Lease Term Insurance: Understanding the Coverage and Benefits
You may want to see also

Credentialing and contracting
Contracting is the process of becoming an in-network provider with insurance companies and establishing the policies for seeing and filing claims for members. It is recommended to apply to several carriers at once, as processing times vary and can take from one month to several months. A contract will be sent to the dietitian to sign, outlining the terms, conditions, and fees that the dietitian agrees to once they become credentialed as an in-network provider. It is important to note that contract rates are private and unique to a healthcare provider, and they may be determined by the insurance payer without negotiation. However, it is possible to request a fee schedule and negotiate reimbursement rates in some cases.
The Mystery of HO-1733: Unraveling the Intricacies of Insurance Terminology
You may want to see also

CPT and diagnosis codes
CPT codes, or Current Procedural Terminology codes, are used to identify the services provided by a healthcare professional. CPT codes are different from ICD-10 codes, which are used to describe a medical diagnosis. CPT codes are procedure codes that describe the service rendered by the healthcare professional.
The three most common medical nutrition therapy (MNT) CPT codes used by dietitians are:
- 97802: For an initial assessment, face-to-face, 15 minutes per unit. This code is used for the first visit with a qualified nutrition professional.
- 97803: For a follow-up visit or reassessment, face-to-face, 15 minutes per unit. This code is for subsequent visits after the initial visit.
- 97804: For a group visit (2 or more individuals), 30 minutes per unit. This code is used when two or more patients meet with the nutritionist.
These CPT codes are applicable for both in-person and telehealth nutrition counselling sessions. When billing for telehealth services, the Place of Service Code should be changed to 02 to indicate telehealth. Additionally, a modifier code may be required, with 95 being the most commonly used for Medical Nutrition Therapy (MNT) codes.
It is important to note that CPT codes are determined by the type of visit, and only one CPT code is used per visit. The reimbursement rate for these CPT codes may vary depending on the insurance company and the provider's contract.
When filing an insurance claim, it is crucial to include the correct CPT codes in the designated section of the CMS 1500 form, usually in section 24d "Procedures, Services, or Supplies." Incomplete or incorrect claims may be denied by the insurance provider.
In addition to CPT codes, diagnosis codes, or ICD-10 codes, are also used on insurance claims. These codes identify the patient's medical diagnosis and are determined by a physician. A common ICD-10 code for dietary counselling and surveillance is Z71.3.
Understanding Insurance Billing for Massages: A Comprehensive Guide
You may want to see also

Telehealth billing tips
Understanding Insurance Reimbursement
The process of understanding insurance reimbursement can be complex, and the credentialing process can be daunting. Familiarise yourself with important terminology and steps to ensure you can move through credentialing smoothly and obtain the best reimbursement rates for your nutrition services.
Fee Schedules
A "fee schedule", or "contract rates", is a list of fees used by insurance payers to compensate doctors or other wellness providers/suppliers. Dietitians are considered "fee-for-service" providers, meaning they are reimbursed by insurance payers after providing a service to clients. Each insurance payer creates its own fee schedule, and these vary for each insurance company.
CPT and HCPCS Codes
When billing insurance payers, you will need to indicate a billing code on your CMS1500 claim for each client encounter. CPT (Current Procedural Terminology) codes are set by the American Medical Association and offer a uniform language for coding medical services and procedures. CPT codes are five-digits and can be numeric or alphanumeric.
HCPCS (Healthcare Common Procedure Coding System) codes are used for billing Medicare and Medicaid patients and represent procedures, supplies, products and services provided.
Telehealth CPT Codes
Some CPT codes are specific to telehealth services. For example, CPT codes 99441, 99442, 99443, G0438 and G0439 are used for telephone evaluation and management services.
Telehealth and Insurance Coverage
Due to the variance in state telehealth laws, there is inconsistency in how insurance companies define and reimburse for telehealth services. Traditionally, telehealth has been used by medical doctors, dermatologists and psychiatrists. Virtual nutrition care is a relatively new service being considered and approved by insurance providers.
In-Network Coverage
In-network coverage depends on each client's insurance plan, state, and each provider's enrolment status. Some insurance companies that cover telehealth services include UnitedHealthcare, Cigna, Aetna, Anthem Blue Cross Blue Shield and Medicare.
Questions to Ask Insurance Companies
- Is my provider in-network or out-of-network? Do I have out-of-network benefits?
- Are telehealth visits covered for CPT codes 97802 (initial consultations) and 97803 (follow-up consultations)?
- Does my policy cover preventative nutrition counselling?
- Does my policy cover medical nutrition therapy for a specific disease or condition?
- Do I need a referral from my primary care physician?
- Does my plan have a limit to the number of visits covered per calendar year?
- Will I have to pay co-insurance, a co-pay, or a deductible before my nutrition counselling session is covered?
Insurance Classification Conundrum: Understanding the Nuanced World of Amateur Pilot Insurance
You may want to see also

Legal considerations
- Licensing and Credentialing: To provide telehealth services across state lines, practitioners must navigate complex licensing requirements. Each state has its own laws and regulations regarding licensing, and most states require providers to be licensed in the state where the client is located during the encounter. This can be challenging for practitioners who want to offer telehealth services to clients in multiple states. Some states have interstate licensure compacts that allow providers to practice across state lines more easily. It's important to review the regulations in the relevant states and ensure compliance with all licensing requirements.
- Informed Consent: Obtaining informed consent from clients is crucial for telehealth services. Informed consent involves communicating the benefits and risks associated with participating in telehealth services, ensuring that clients make informed decisions. Some states may have specific informed consent requirements, such as written forms or oral acknowledgments.
- Reimbursement and Payment Policies: Understanding reimbursement policies is essential for billing insurance for telehealth nutrition counseling. Both federal and state-level policies exist, and they vary across states and insurance providers. It's important to know which services are covered by Medicare, Medicaid, and private insurance companies. Additionally, the reimbursement rates and payment procedures can differ, so it's crucial to be familiar with the policies of the relevant insurance companies.
- Billing Codes and Modifiers: When billing insurance companies, it's important to use the correct billing codes and modifiers. Common billing codes for nutrition services include CPT codes (Current Procedural Terminology) and HCPCS codes (Healthcare Common Procedure Coding System). Modifiers such as "DR" (disaster-related) and "CR" (catastrophe-related) may be necessary during emergency situations like the COVID-19 pandemic.
- Data Security and Privacy: Protecting patient health information is critical. Telehealth providers must ensure compliance with the Health Insurance Portability and Accountability Act (HIPAA) and other relevant data security regulations. This includes using HIPAA-compliant telehealth platforms and safeguarding patient data from malware and hacker attacks.
- Malpractice and Liability Insurance: Telehealth providers should have adequate malpractice insurance coverage that extends to the states in which they practice. It's important to confirm with insurance carriers that their coverage includes telehealth services. Additionally, consider cyber liability coverage to protect against data breaches and hacking.
Unraveling the Maryland Bridge Insurance Billing Process
You may want to see also
Frequently asked questions
CPT codes are set by the American Medical Association and are used for coding medical services and procedures. CPT codes for nutrition services include:
- 97802 – medical nutrition therapy; initial assessment and intervention, individual, face-to-face with the patient; each 15 minutes
- 97803 – medical nutrition therapy; re-assessment and intervention, individual, face-to-face with the patient; each 15 minutes
- 97804 – medical nutrition therapy; group (2 or more individuals); each 30 minutes
HCPCS codes are used for billing Medicare and Medicaid patients and include:
- G0270 – medical nutrition therapy; reassessment and subsequent intervention(s)
- G0271 – medical nutrition therapy; reassessment and subsequent intervention(s), group (2 or more individuals)
- G0108 – DSMT (diabetes self-management training), individual session, each 30 minutes
Accepting insurance for nutrition counseling can increase the number of clients you can see, as it makes your services more affordable and accessible. It can also lead to referrals from doctors and help you grow your practice.
First, verify your client's insurance coverage and eligibility for nutrition counseling services. Then, determine the CPT and HCPCS codes relevant to the services provided. Submit a claim to the insurance company using the CMS-1500 form, indicating the CPT and HCPCS codes. Finally, follow up with the insurance company to ensure the claim is processed correctly and receive reimbursement.