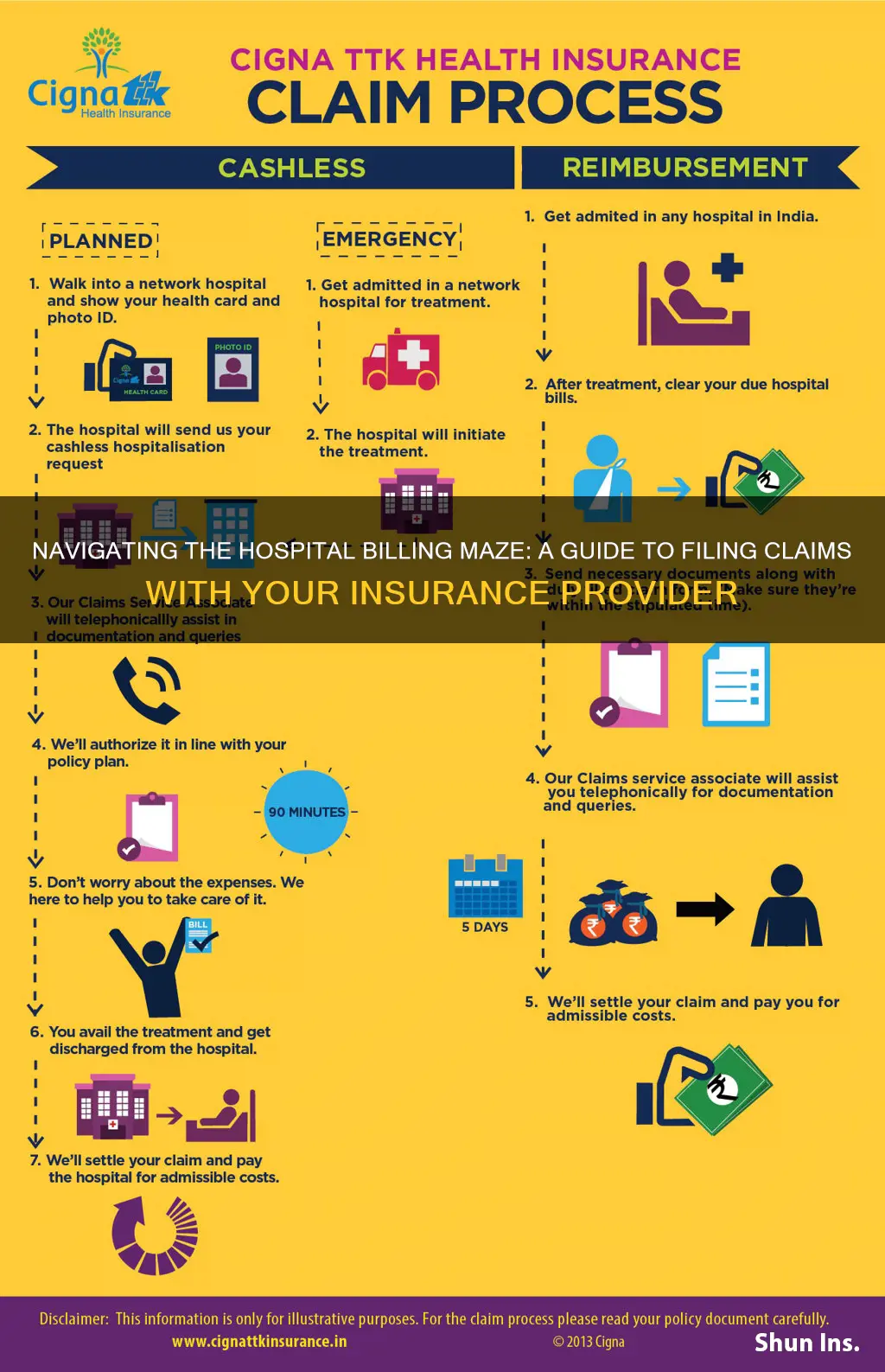
If you've received a hospital bill, the last thing you want is to be faced with complicated jargon and a mountain of paperwork. It's important to know how to file a claim with your insurance company to avoid this. The process can reimburse you for any visits you've paid for and ensure your medical bills are paid promptly. Here's a step-by-step guide to help you file a hospital bill with your insurance company.
| Characteristics | Values |
|---|---|
| What to do when you receive a hospital bill | Check if the bill contains the words "insurance pending" or any other indication that the hospital has submitted the bill to the insurance company. If not, contact the hospital and ask them to bill your insurance company. If they refuse, fill out a reimbursement form and send it to your insurance company. |
| How to submit an insurance claim | 1. Collect itemized receipts from your medical provider. 2. Complete a claim form with personal information, insurance information, reason for your visit, and provider information. 3. Make copies of all documents. 4. Review the paperwork, call your insurance company, and send the claim form and accompanying paperwork. |
| Protection from unexpected bills | The No Surprises Act protects people from unexpected out-of-network medical bills for emergency room visits and non-emergency care related to a visit to an in-network hospital. State and federal laws also protect against surprise billing when receiving emergency care or when receiving care from an out-of-network provider at an in-network facility. |
What You'll Learn

Check for insurance pending on the bill
When you receive a hospital bill in the mail, the first thing to do is check whether it contains the words "insurance pending" or any other indication that the hospital has already submitted the bill to your insurance company. If the bill is pending insurance, it means that the hospital or doctor's office has sent the bill to your insurance company, and you don't need to do anything further at this stage. The insurance company will process the claim and pay the doctor or hospital directly for the services covered under your plan.
If the bill does not indicate that it is pending insurance, you should call the hospital or doctor and ask them to bill your insurance company, providing them with the details from your insurance card or certificate. If they refuse or are unable to do so, you may need to take further steps, such as filling out a reimbursement form and submitting it to your insurance company.
It's important to keep track of your medical bills and insurance claims to ensure that you are not overcharged or billed for services that should be covered by your insurance. Keep all documentation organised and easily accessible, and always review your bills and statements carefully. If you have any questions or concerns about your bill, don't hesitate to contact your insurance company or seek advice from a relevant organisation or expert.
In the case of surprise billing, where you receive a bill from an out-of-network provider or facility, you are protected by state and federal laws, such as the No Surprises Act, which prevent you from being charged for unexpected out-of-network medical expenses in certain situations. If you believe you have been wrongly billed, you can contact the provider or facility and dispute the charge.
Osteopathic Doctors and Insurance Billing: Understanding the Process
You may want to see also

Ask the hospital to bill your insurance company
If you receive a hospital bill in the mail, the first thing to do is to check if it contains the words "insurance pending" or some other indication that the hospital has already submitted the bill to your insurance company. If it doesn't, you should call the hospital and ask them to bill your insurance provider. Provide them with the information on your insurance card or certificate.
Asking the hospital to bill your insurance company is a straightforward process. First, contact the hospital's billing department by phone and inform them that you would like them to bill your insurance company directly. Have your insurance information ready, including the name of your insurance company, your insurance plan or policy number, and any relevant group numbers. You may also need to provide personal information such as your full name, address, and date of birth. Additionally, be prepared to give details about the reason for your hospital visit or treatment.
It is important to note that, in some cases, the hospital may not be able to bill your insurance company directly. This could be due to various reasons, such as being out of your insurance network or other administrative constraints. In such situations, you may need to take additional steps to ensure your insurance company receives the bill and processes your claim.
If the hospital refuses or is unable to send the bill to your insurance company, don't panic. You can still take matters into your own hands and submit the claim yourself. This typically involves filling out a claim form provided by your insurance company and attaching the itemized bill or receipts from the hospital. Keep in mind that it is always a good idea to make copies of all the documents for your records before submitting them.
By following these steps and communicating your needs clearly, you can effectively navigate the process of asking the hospital to bill your insurance company. Remember to stay organized, keep track of important documents, and don't be afraid to reach out to your insurance provider or seek additional assistance if needed.
COBRA Coverage: Understanding Your Insurance Continuation Rights
You may want to see also

Fill out a reimbursement form
Filling out a reimbursement form is a careful process, especially if it's your first time. Here is a step-by-step guide to help you fill out a reimbursement form and raise a claim request smoothly and successfully.
Step 1: Collect Your Itemized Receipts
To file a claim, you need to first obtain an itemized bill from your doctor or medical provider. This bill will list every service you received, along with the cost and a special code that the insurance company will need to pay your claim. Getting these receipts is easy – simply call your provider and let them know you are filing an insurance claim.
Step 2: Complete the Reimbursement Form
The reimbursement form is a document that tells your insurance company more details about the accident or illness in question. This will help them determine if the expenses you are claiming for are covered under your insurance plan. You can usually find the reimbursement form on your insurance company's website. The form will have instructions for completing it and directions on how and where to send it.
Typical sections of a reimbursement form include:
- Personal information, such as your name, address, and date of birth
- Insurance information, such as a policy and group number
- Reason for your visit, including background information about your condition
- Provider information, including the doctor's name and address
- Out-of-pocket expenses that you have already paid
Step 3: Make Copies of Your Documents
Before sending your reimbursement form to your insurance company, make at least one copy of your entire claim. Keep an extra copy of the completed form, as well as your receipts, in case there is a complication with your claim.
Step 4: Review, Call and Send
If possible, send your claim by email or fax, as this will be quicker, and you can keep the original documents. Call your insurance company and let them know you will be sending in a claim form. Review the paperwork you are about to send and ask if there are any additional documents that need to be sent.
Once you are certain you have everything in order, send out your reimbursement form and accompanying paperwork to your insurance company. If you need an address to send it to, check your claim form. Most of the time, you will be expected to mail in your claim, but sometimes you can submit your documents by email or fax.
Step 5: Follow Up
Keep an eye on the calendar and note the claim date that your insurance company gave you when you called. If you don't receive payment for your claim within the given timeframe, contact your insurance company. When you speak to someone, make sure to write down the date, time, and the name(s) and job titles of the people you speak to, to create a paper trail. Don't be afraid to follow up with your insurance company after your claim has been submitted to ensure they have all the necessary documents and that they are filled out correctly.
Additional Tips:
- If you have already paid for your treatment, the insurance company or healthcare provider will reimburse you for those services covered under your claim. If you have not paid for your treatment, the insurance company will pay the doctor/hospital directly.
- If your claim is denied, don't panic. This happens a lot more than you'd think. There are many reasons insurance companies deny claims, including coding errors, failure to get prior authorization, missing or incorrect information, and treatment deemed medically unnecessary or experimental. There is always an appeals process, so make sure you have all your records in order and contact your healthcare provider if necessary.
- If your insurance company denies your claim because the treatment is deemed not medically necessary, you will likely need to involve your healthcare provider. Your doctor can set up a peer-to-peer review, where they speak with the insurance company's doctor to explain the medical necessity of the treatment or procedure.
- If you are filing for reimbursement for psychotherapy, you will need to include the diagnosis code (“ICD”) and the procedure code (“CPT”) on your reimbursement form.
Understanding Draft Authority: Unraveling the Complexities of Insurance Terminology
You may want to see also

Attach itemised bill to the claim form
To file a hospital bill on insurance, you will need to obtain an itemised bill from your healthcare provider. This will list every service you received, along with the cost and a special code that the insurance company will need to process your claim. To obtain this, simply call your provider and inform them that you are filing an insurance claim. They will need some basic information, such as your full name and date of service, and should then send you your itemised receipts promptly.
Once you have your itemised bill, you can attach it to your claim form. This is a document that tells your insurance company more about the accident or illness in question and helps them determine whether the expenses you are claiming for are covered by your insurance plan. You can usually find the claim form on your insurance company's website, and they may also allow you to file the claim online. However, you should be prepared to print the form and mail it in.
The claim form will ask for personal information, such as your name, address, and date of birth, as well as insurance information, such as your policy and group number. You will also need to provide the reason for your treatment, including background information about your condition, and the name and address of your doctor or medical provider.
In addition to the itemised bill, it is a good idea to make copies of all relevant documents and keep them in a file specifically marked for your claim. This includes the completed claim form and any other receipts or paperwork related to your treatment. Having all of this information in one place will make it easier to refer back to if there are any complications or disputes with your claim.
Finally, before submitting your claim, review all the paperwork and call your insurance company to let them know that you will be sending in a claim form. This is also a good opportunity to ask if there are any additional documents they need and how long it will take to process your claim.
The Intricacies of Insurance Endorsements: Unraveling the Added Layer of Protection
You may want to see also

Keep copies of all documents
Keeping copies of all documents is an essential step in the process of filing a hospital bill insurance claim. This is a precautionary measure that ensures you have everything you need in case there is a complication with your claim. Here are some reasons why keeping copies of all documents is crucial:
- To Have a Record for Reference: Keeping copies of documents allows you to refer back to the specifics of your claim. This includes details such as the services received, corresponding costs, and special codes that the insurance company needs to process your claim. Having a copy allows you to review and confirm the accuracy of the information submitted.
- To Facilitate Follow-up and Dispute Resolution: In the event of a dispute or if your claim is denied, having copies of all documents enables you to effectively follow up with the insurance company. You can refer to the copies to identify any discrepancies or missing information and take the necessary corrective actions. Copies of documents create a paper trail, which can be invaluable if you need to escalate or dispute a claim.
- To Comply with Record-Keeping Requirements: Depending on the type of insurance policy and applicable laws, there may be specific requirements for retaining records. For example, for tax purposes, businesses or self-employed individuals may need to keep insurance records for several years. In the US, state laws generally require insurance agents to retain customer policy records for around 6-7 years. Therefore, it is prudent to keep copies of all documents to comply with any applicable record-keeping obligations.
- To Ensure a Smooth Claims Process: By keeping copies of all documents, you can easily provide additional information or clarify any questions that may arise during the claims process. This helps to expedite the processing of your claim and reduces the likelihood of delays caused by missing or unclear information.
- To Protect Yourself in Case of Loss or Misplacement: Unfortunately, insurance claim forms can sometimes get lost or misplaced. By keeping your own copies, you ensure that you have a backup set of documents. This is especially important if the original documents are lost by the insurance company or healthcare provider, as it can be challenging to obtain duplicates of certain records.
When keeping copies of documents, make sure to maintain both digital and hard copies. Store hard copies in a secure, climate-controlled environment to prevent damage and consider using a waterproof and fireproof safe for added protection. For digital copies, utilize both cloud-based and drive-based storage methods to ensure redundancy in case one storage method fails.
Updating Term Insurance: Changing Nominees and Ensuring Peace of Mind
You may want to see also
Frequently asked questions
First, check if the bill contains the words "insurance pending" or any other indication that the hospital has submitted the bill to your insurance company. If it does not, call the hospital and ask them to bill your insurance company. Provide them with the information on your insurance card. If they refuse or are unable to do this, you will need to fill out a reimbursement form and send it to your insurance company.
To file a claim, you will need to obtain an itemized bill from your doctor or medical provider, listing every service you received, along with the cost and a special code. You will then need to complete a claim form, providing personal information, insurance information, details of your treatment, and any out-of-pocket expenses. Make at least one copy of your claim and supporting documents before sending them to your insurance company.
There are several reasons why insurance claims are denied, including coding errors, failure to obtain prior authorization, missing or incorrect information, treatment deemed medically unnecessary, or treatment not covered by your plan. If your claim is denied, don't panic. Contact your insurance company and ask about the appeals process. Make sure you have all your records, including documentation of any phone calls, in order. If the denial is due to your insurance company deeming the treatment medically unnecessary, you may need to involve your healthcare provider to set up a peer-to-peer review.