If you are a Presbyterian Health Plan member, it is important to notify the health plan of any changes to your name, address, phone number, marital status, or newborns that may affect your eligibility. This notification must be made within 31 days of the change. To do this, you can contact the Presbyterian Customer Service Center and request a Coordination of Benefits form.
| Characteristics | Values |
|---|---|
| Time to notify of name change | 31 days |
What You'll Learn

Notify Presbyterian of name changes within 31 days
It is important to notify Presbyterian of any name changes within 31 days. This is because your name is included on your member ID card, which serves as proof of your health insurance with Presbyterian.
To update your name on your insurance, you will need to contact the Presbyterian Customer Service Center. You can do this by calling 1-800-659-8331 or by sending an email to [email protected]. The Customer Service Center operates from Monday to Friday, 7:00 a.m. to 6:00 p.m.
When contacting the Customer Service Center, you will need to provide your previous name and your new name, as well as any other relevant information or documentation to support your name change. It is important to have your member ID card handy when making this call, as you may be asked to provide your member number or other information from the card.
If you have moved to a new address within the same state, you can update your address by logging into your HealthCare.gov account, choosing the application you want to update, clicking "Report a Life Change," and then following the prompts to report your change of address. Alternatively, you can contact the Marketplace Call Center or find someone in your community to help you update your application in person.
It is important to keep your information up to date with your insurance provider to ensure that you continue to receive the benefits and coverage you need.
Understanding the Fundamentals of Minimum Sum Assured in Term Insurance
You may want to see also

Update your ID card
Updating your ID card is simple and can be done in a few different ways. Firstly, you can log in to your myPRES account and select MyIDCard to print, fax, or email your ID card. Alternatively, if you are at a provider's office, they should be able to access your health plan information with your social security number. If you need to replace, view, or obtain a copy of your member ID card, you can log in to myPRES or call the Presbyterian Customer Service Center to request a replacement.
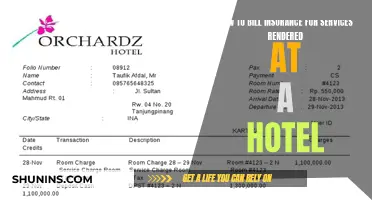
Your member ID card is used as proof of your health insurance with Presbyterian. It is important to keep your member ID card with you when you need healthcare at medical facilities or pharmacies. You can print a temporary ID card on myPRES. It is also important to take your ID card with you when you travel, as it contains important information and phone numbers you may need in an emergency.
Your ID card contains helpful information for both you and your providers. This includes your name, your unique member ID number, the effective date of your health insurance coverage, your group number (specific to your plan type or employer), and the name of your health plan. If you see the Aetna logo on your card, this means you can access the Aetna provider network if you need care outside of New Mexico. Check your plan documents or call customer service for details.
Broker Change: Insurance Simplified
You may want to see also

Update your application online
To update your application online, log in to your HealthCare.gov account. From there, you can choose the application you want to update. Click "Report a Life Change" on the left-hand menu. Read through the list of changes and click "Report a Life Change" to get started. Next, select the kind of change you want to report. You can then navigate through your application and report any changes to your income, household members, address, new health coverage offers, and other information. After you're done, you'll get new eligibility results explaining your options to change plans.
It's important to complete all steps on your To-Do List for your changes to take effect. This includes, if given the option, completing your enrollment.
Note that you can also update your application by phone or in person, but not by mail.
Haven Insurance: Updating Your Address, Securing Your Coverage
You may want to see also

Update your application by phone
To update your application by phone, you can contact the Marketplace Call Center and have a representative walk you through the process of updating your application. This is one of three ways to update your application, the other two being online or in person.
When updating your application, you will need to navigate through your existing application and make edits. You will then be prompted to re-submit your application. This will not cause any disruption to your current coverage.
During the process, you will be asked to report a life change, which could include a name change. You will then be able to select the kind of change you want to report and navigate through your application to report any changes to your income, household members, address, new health coverage offers, and other information.
After you have completed all the steps, you will receive new eligibility results explaining your options to change plans.
Updating Your Last Name on UMPC Insurance: A Step-by-Step Guide
You may want to see also

Update your application in-person
To update your application in person, you can find someone in your community who can work with you to help make changes to your application. This could be a friend, family member, or someone from a community centre.
To do this, you will need to navigate through your existing application and make edits. When you do, you will be prompted to re-submit your application. This is normal and will not cause any disruption to your current coverage.
Log in to your HealthCare.gov account and choose the application you want to update. Click "Report a Life Change" on the left-hand menu and read through the list of changes. Click "Report a Life Change" to get started and select the kind of change you want to report.
You will then need to navigate through your application and report any changes to your income, household members, address, new health coverage offers, and other information. Once you are done, you will get new eligibility results explaining your options to change plans.
It is important to complete all steps on your To-Do List for your changes to take effect. This may include completing your enrollment if you are given the option.
Understanding the Basics of Standard Term Insurance: A Comprehensive Guide
You may want to see also
Frequently asked questions
Contact the Presbyterian Customer Service Center and request a Coordination of Benefits form. You can also inform them of any additional healthcare coverage you have.
Please allow up to 15 business days to receive your new card in the mail.
You can log in to your myPRES account and select MyIDCard to print, fax, or email your ID card. Alternatively, your provider's office should be able to access your health plan information with your social security number.
Send the Add Dependent form and a copy of a document that shows proof of the date of birth or a legal document such as a birth certificate.
Commercial members must notify the health plan of changes within 31 days.