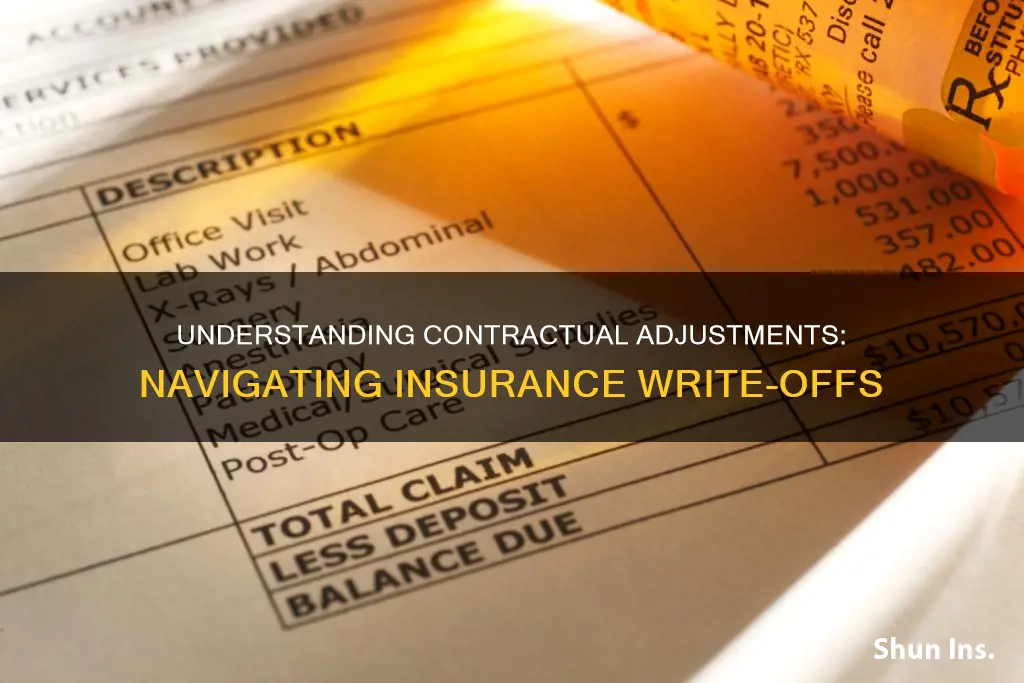
Contractual adjustments are a common feature of the billing system, where a doctor or hospital must write off a portion of a patient's bill due to billing agreements with the insurance company. This is typically the difference between the amount charged by the provider and the amount agreed to be paid by the insurance company, known as the allowable amount. For example, if a provider charges $100 for a service, and the insurance company's allowance is $80, the remaining $20 will be written off as a contractual adjustment. This ensures that the provider receives a significant portion of their fee, which may otherwise be unaffordable for patients without insurance. It is important for patients and hospitals to understand contractual adjustments to avoid any legal or ethical issues, as hospitals are prohibited from charging patients the remaining amount in the case of insured patients.
| Characteristics | Values |
|---|---|
| Definition | A contractual adjustment is a part of a patient's bill that a doctor or hospital must write off because of billing agreements with the insurance company. |
| Other terms | Billing amount, maximum allowable charge, write-off |
| Billing amount | The total bill charged by a hospital to a patient for the services and care they received. |
| Maximum allowable charge | The amount fixed and usually paid by the insurance company. |
| Contractual adjustment calculation | Difference between the billing amount and the maximum allowable charge. |
| Patient with insurance | The hospital cannot charge the patient the remaining amount after the maximum allowable charge. |
| Patient without insurance | The patient must pay the full fee if they do not have an insurance contract. |
| Group codes | CO, OA, PI, PR |
| CO – Contractual Obligations | Used when a joint contractual agreement between the payer and payee, or a regulatory requirement, resulted in an adjustment. |
| OA – Other Adjustments | Used when no other group code applies to the adjustment. |
| PI – Payer Initiated Reductions | Used when, in the opinion of the payer, the adjustment is not the patient's responsibility, but there is no contract between the provider and the payer. |
| PR – Patient Responsibility | Used when the adjustment is an amount that should be billed to the patient or insured, typically for deductible and copay adjustments. |
What You'll Learn
- Contractual adjustments are the most common type of adjustment
- They are the difference between the billing amount and the maximum allowable charge
- Hospitals are prohibited from charging patients the remaining amount
- Contractual adjustments are only made on services covered by the insurance company
- Group codes are used for claim adjustments

Contractual adjustments are the most common type of adjustment
In health insurance, contractual adjustments are applied when an insured person is covered by an individual or group health plan involving a network of providers contracted by the insurer. The insurer, insured, and providers are the three parties in the insurance process, and each participant generally benefits from the established provider network arrangement.
Healthcare providers often deal with multiple parties during the billing process, including patients, third-party insurers, and government programs. When estimating ultimate collections, providers consider both contractual allowances (adjustments) and bad debt allowances. Contractual allowances represent adjustments to gross revenue based on contractual agreements with insurers or government programs, while bad debt allowances are estimates of uncollectible net revenue based on historical patient/payer payment trends.
It is important for patients and hospitals, especially their billing offices, to understand contractual adjustments to avoid legal or ethical issues. Hospitals must not charge patients the remaining amount after a contractual adjustment, provided the patient has an agreement with the insurance company. Outsourcing medical billing services from a specialised company can help hospitals avoid mistakes and legal issues related to contractual adjustments.
Navigating the Path to Becoming an Insurance Adjuster in Oklahoma
You may want to see also

They are the difference between the billing amount and the maximum allowable charge
A contractual adjustment is a difference between the billing amount and the maximum allowable charge. It is a common type of adjustment, often occurring when there is a discrepancy between what a provider charges for healthcare services and what an insurance company has decided to pay for that service.
The billing amount is the total bill charged by a hospital for the services and care provided. This amount is always more than the maximum allowable charge. The maximum allowable charge is a fixed amount, usually paid by the insurance company, to compensate the insured patient for the services they have received. This amount is set beforehand and is lower than the billing amount.
When a patient has an insurance policy, the Explanation of Benefits (EOB) outlines the maximum allowable charge for each medical service. This contractual agreement between the provider and the insurer ensures that the patient is not overcharged and prevents fraud in billing.
For example, if a hospital charges a total of $100 for a service, and the maximum allowable charge according to the insurance company is $80, the patient will pay their portion of the contracted rate, and the remaining $20 will be adjusted off the patient's account as a contractual adjustment.
Contractual adjustments are an important metric in healthcare revenue cycle management, helping providers understand how much revenue is lost due to these adjustments.
Understanding the Flexibility of Insurance Quotes: Are They Set in Stone?
You may want to see also

Hospitals are prohibited from charging patients the remaining amount
In simple terms, it is an amount reduced from the medical bill because the patient has a contract with the insurance company. Providers charge more for services than what the insurance company agrees to pay, and the amount paid by the insurance is known as an allowable amount. The extra amount that the provider charges is taken care of by the insurance company and is reduced from the final amount. This happens because the patient has a contract or billing agreement with the insurance company, which has reduced the extra amount charged by the provider.
For example, if a provider charges $100 for a certain service, and the contracted rate between the insurance company and the provider for this service is $80, with the insurer paying $64 (80%) and the remaining 20% of the contracted rate amount paid by the patient, the $20 difference between the $100 charged by the provider and the $80 collected is adjusted off the patient account as a contractual adjustment.
It is important to note that contractual adjustments are only made on services covered by the insurance company. If a patient requires a service that is not covered by the insurance company, they will have to pay the full amount charged by the medical provider with no contractual adjustment to limit the cost.
In the context of hospital billing, hospitals are prohibited from detaining patients who are unable to pay their hospital bills. This is in accordance with laws such as the Republic Act No. 9439 in the Philippines, which states that it is unlawful for any hospital to detain patients who have fully or partially recovered or who may have died due to non-payment of hospital bills or medical expenses. Patients who are financially incapable of settling their hospital bills have the right to demand the issuance of the corresponding medical certificate and other necessary documents for their release upon the execution of a promissory note covering the unpaid obligation.
In-House Insurance Adjusters: Walking the Legal Tightrope
You may want to see also

Contractual adjustments are only made on services covered by the insurance company
Contractual adjustments are a common feature of the billing process in the healthcare industry. They occur when there is a difference between the amount a healthcare provider charges for a service and the amount an insurance company has agreed to pay for that service.
When a healthcare provider agrees to accept an insurance plan as payment, they enter into a contractual arrangement with the insurer. This contract will include details such as the amount the insurance company will pay the provider for certain procedures. Providers often charge more for their services than what the insurance company agrees to pay. The amount that is paid by the insurance company is known as the allowable amount. The amount above what the insurance company agrees to pay is a reduction known as a contractual adjustment.
It is important to remember that contractual adjustments are only made on services covered by the insurance company. If a patient requires a service that is not covered by their insurance, they will be responsible for paying the full amount charged by the provider.
For example, if a provider charges $100 for a service, and the contracted rate between the insurance company and the provider for this service is $80, the insurer may pay $64 (80%), with the patient paying the remaining 20% of the contracted rate. The $20 difference between the original charge and the amount paid by the insurance company is adjusted off the patient's account as a contractual adjustment.
Contractual adjustments are beneficial for providers as they ensure that they receive at least a significant portion of their fee. Without insurance, patients may not be able to afford the full cost of the service. By accepting the contracted rates, providers also gain broader access to members of the insurance company.
The Road to Becoming an Automotive Insurance Adjuster: A Comprehensive Guide
You may want to see also

Group codes are used for claim adjustments
Group codes are an essential component of the claim adjustment process, providing clarity and consistency in insurance billing and reimbursement. In this context, group codes refer specifically to Claim Adjustment Group Codes, which are two-letter codes that indicate the reason for a claim adjustment on the insurance Explanation of Benefits. These codes are used to determine responsibility for adjustments and ensure accurate financial transactions between payers and providers.
There are five main Claim Adjustment Group Codes:
- CO - Contractual Obligation: This code is used when an adjustment arises from a contractual agreement between the payer and the payee or due to regulatory requirements. It is considered a write-off for the provider and is typically not billed to the patient.
- CR - Corrections and Reversal: This code is selected when no other group code applies to the adjustment. It indicates a correction or reversal of a prior decision without any financial liability.
- PI - Payer Initiated Reductions: Payers use this code when they believe the patient is not financially responsible for the adjustment, but there is no supporting contract between the provider and the payer.
- PR - Patient Responsibility: This code signifies that the adjustment is an amount to be billed to the patient or secondary insurance. It is commonly used for deductible, coinsurance, and copay adjustments.
- OA - Other Adjustments: The OA code is utilised when no other group code is applicable for the specific adjustment.
Each of these group codes is combined with Claim Adjustment Reason Codes, which provide further detail on the reason for the adjustment. These reason codes can be numeric or alphanumeric and offer specific explanations for the discrepancy between the billed and paid amounts. By utilising both group codes and reason codes, the insurance billing process becomes more transparent and efficient, reducing ambiguity and streamlining administrative tasks.
Navigating the Path to Becoming an Insurance Adjuster in Massachusetts
You may want to see also
Frequently asked questions
A contractual adjustment is a part of a patient’s bill that a hospital must write off because of billing agreements with the insurance company. It is the difference between the billing amount and the maximum allowable charge.
A write-off is an amount that a hospital deducts from a charge and does not expect to collect from the patient. Write-offs are common practice and can be divided into two categories: approved and other write-offs.
Charity write-offs, small balance write-offs, prompt payment discounts, and self-pay discounts are some examples of approved write-offs.
Timely filing write-offs, collection agency write-offs, uncredentialed provider write-offs, and administrative write-offs are some examples of other write-offs.
Contractual adjustments are a type of write-off that occurs due to billing agreements with the insurance company. Write-offs, on the other hand, can occur for various reasons, including contractual adjustments, charity, small balances, and other factors.