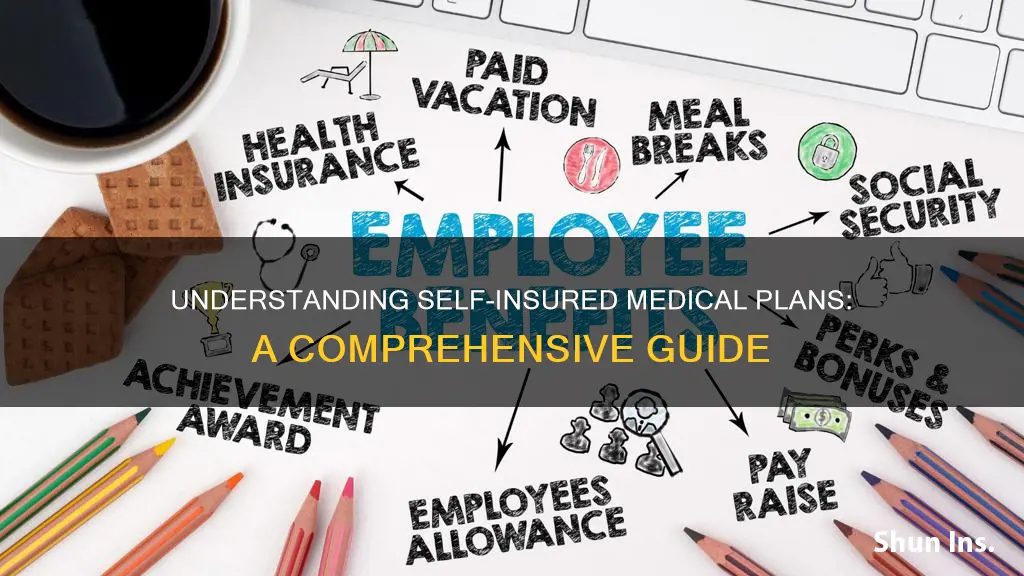
A self-insured health plan is a coverage offered by an employer or association in which the employer takes on the risk involved with providing coverage, instead of purchasing coverage from an insurance company. Self-insured health plans involve employers assuming all financial risk for providing benefits to employees, allowing for more flexibility in plan design and potential cost savings, but also carrying more financial risk and administrative burden.
| Characteristics | Values |
|---|---|
| Self-insured health plans are coverage offered by an employer or association | The employer or association pays for enrollees' medical care directly |
| Self-insured coverage means that the employer or association pays for enrollees' medical care directly | The employer or association pays for enrollees' medical care directly |
| Self-insured health plans can be administered by the employer or association | A third-party administrator (TPA) is often used |
| Self-insured health plans can be administered by the employer or association | The TPA is often a commercial insurance carrier |
| Self-insured health plans are not subject to state insurance regulations | They're regulated at the federal level, under ERISA |
| Self-insured health plans are not subject to state insurance regulations | They're regulated at the federal level, under ERISA |
| Self-insured health plans are not subject to state insurance regulations | They're regulated at the federal level, under ERISA |
| Self-insured health plans are not subject to state insurance regulations | They're regulated at the federal level, under ERISA |
| Self-insured health plans are not subject to state insurance regulations | They're regulated at the federal level, under ERISA |
| Self-insured health plans are not subject to state insurance regulations | They're regulated at the federal level, under ERISA |
What You'll Learn

Employers take on risk with self-insured health plans
A self-insured health plan is a coverage offered by an employer or association in which the employer takes on the risk involved with providing coverage, instead of purchasing coverage from an insurance company. Self-insured coverage means that the employer or association pays for enrollees' medical care directly.
Self-insured health plans are not subject to state insurance regulations. Instead, they're regulated at the federal level, under ERISA. Self-insured plans are, however, subject to various aspects of several federal laws, including the ACA, COBRA, HIPAA, and the No Surprises Act.
Self-insured health plans involve employers assuming all financial risk for providing benefits to employees, allowing for more flexibility in plan design and potential cost savings, but also carrying more financial risk and administrative burden.
Self-insured health plans can be administered by the employer or association, but it's common for a third-party administrator (TPA) to be used. The TPA is often a commercial insurance carrier, so the employees' ID cards might have the name of an insurance carrier on them, and the plan might use that insurer's provider network.
Self-insured health plans are different from fully insured plans where the employer contracts an insurance company to cover the employees and dependents. In self-funded health care, the employer assumes the direct risk for payment of the claims for benefits. The terms of eligibility and covered benefits are set forth in a plan document which includes provisions similar to those found in a typical group health insurance policy.
Understanding Medical Insurance: The Three Essential Coverages Explained
You may want to see also

Self-funded health care uses company funds
Self-funded health care, also known as Administrative Services Only (ASO), is a self-insurance arrangement in the United States whereby an employer provides health or disability benefits to employees using the company's own funds. This is different from fully insured plans where the employer contracts an insurance company to cover the employees and dependents. In self-funded health care, the employer assumes the direct risk for payment of the claims for benefits. The terms of eligibility and covered benefits are set forth in a plan document which includes provisions similar to those found in a typical group health insurance policy.
Self-insured health plans are not subject to state insurance regulations. Instead, they're regulated at the federal level, under ERISA. So for example, if a state requires health plans to cover services like bariatric surgery or infertility treatment, or add additional state continuation after COBRA is exhausted, those requirements would not apply to self-funded health plans. Self-insured plans are, however, subject to various aspects of several federal laws, including the ACA, COBRA, HIPAA, and the No Surprises Act.
Self-insured coverage means that the employer or association pays for enrollees' medical care directly. Self-insured health plans can be administered by the employer or association, but it's common for a third-party administrator (TPA) to be used. The TPA is often a commercial insurance carrier, so the employees' ID cards might have the name of an insurance carrier on them, and the plan might use that insurer's provider network.
Self-insured health plans involve employers assuming all financial risk for providing benefits to employees, allowing for more flexibility in plan design and potential cost savings, but also carrying more financial risk and administrative burden.
Self-insured health plans are coverage offered by an employer or association in which the employer (or association) takes on the risk involved with providing coverage, instead of purchasing coverage from an insurance company.
Uncover the Truth: Medical Insurance and Laser Eye Surgery
You may want to see also

HRAs offer benefits without financial risk
Self-insured health plans are coverage offered by an employer or association in which the employer takes on the risk involved with providing coverage, instead of purchasing coverage from an insurance company. In a self-insured plan, the employer or association pays for enrollees' medical care directly.
Self-insured health plans can be administered by the employer or association, but it's common for a third-party administrator (TPA) to be used. The TPA is often a commercial insurance carrier, so the employees' ID cards might have the name of an insurance carrier on them, and the plan might use that insurer's provider network.
Self-insured health plans are not subject to state insurance regulations. Instead, they're regulated at the federal level, under ERISA. So for example, if a state requires health plans to cover services like bariatric surgery or infertility treatment, or add additional state continuation after COBRA is exhausted, those requirements would not apply to self-funded health plans. Self-insured plans are, however, subject to various aspects of several federal laws, including the ACA, COBRA, HIPAA, and the No Surprises Act.
Self-insured health plans involve employers assuming all financial risk for providing benefits to employees, allowing for more flexibility in plan design and potential cost savings, but also carrying more financial risk and administrative burden.
Health reimbursement arrangements (HRAs) offer the benefits of a self-insured plan without the financial risk or administrative burden.
Dental Implants: Unlocking Coverage Secrets with Medical Insurance
You may want to see also

Self-insured plans not subject to state regulations
Self-insured health plans are not subject to state insurance regulations. Instead, they are regulated at the federal level, under the Employee Retirement Income Security Act of 1974 (ERISA). This means that if a state requires health plans to cover services like bariatric surgery or infertility treatment, or add additional state continuation after COBRA is exhausted, those requirements would not apply to self-insured health plans.
Self-insured plans are, however, subject to various aspects of several federal laws, including the ACA, COBRA, HIPAA, and the No Surprises Act.
Self-insured health plans are coverage offered by an employer or association in which the employer (or association) takes on the risk involved with providing coverage, instead of purchasing coverage from an insurance company.
Self-insured coverage means that the employer or association pays for enrollees' medical care directly. Fully insured coverage means that health insurance is being purchased from an insurance company (either by an employer or by an individual) and the insurance company will be the entity responsible for paying for medical care.
Self-insured health plans can be administered by the employer or association, but it's common for a third-party administrator (TPA) to be used. The TPA is often a commercial insurance carrier, so the employees' ID cards might have the name of an insurance carrier on them, and the plan might use that insurer's provider network.
Self-insured health plans involve employers assuming all financial risk for providing benefits to employees, allowing for more flexibility in plan design and potential cost savings, but also carrying more financial risk and administrative burden.
Breast Pumps and Insurance: Unlocking Coverage for New Moms
You may want to see also

Self-insured plans regulated at the federal level
Self-insured health plans are not subject to state insurance regulations. Instead, they're regulated at the federal level, under ERISA. This means that if a state requires health plans to cover services like bariatric surgery or infertility treatment, or add additional state continuation after COBRA is exhausted, those requirements would not apply to self-funded health plans.
Self-insured plans are, however, subject to various aspects of several federal laws, including the ACA, COBRA, HIPAA, and the No Surprises Act.
Self-insured health plans are coverage offered by an employer or association in which the employer (or association) takes on the risk involved with providing coverage, instead of purchasing coverage from an insurance company.
Self-insured coverage means that the employer or association pays for enrollees' medical care directly. Fully insured coverage means that health insurance is being purchased from an insurance company (either by an employer or by an individual) and the insurance company will be the entity responsible for paying for medical care.
Self-insured health plans can be administered by the employer or association, but it's common for a third-party administrator (TPA) to be used. The TPA is often a commercial insurance carrier, so the employees' ID cards might have the name of an insurance carrier on them, and the plan might use that insurer's provider network.
Self-funded health care, also known as Administrative Services Only (ASO), is a self-insurance arrangement in the United States whereby an employer provides health or disability benefits to employees using the company's own funds. This is different from fully insured plans where the employer contracts an insurance company to cover the employees and dependents. In self-funded health care, the employer assumes the direct risk for payment of the claims for benefits. The terms of eligibility and covered benefits are set forth in a plan document which includes provisions similar to those found in a typical group health insurance policy.
Navigating Insurance for Pre-Existing Conditions: Finding the Right Coverage
You may want to see also
Frequently asked questions
A self-insured medical plan is a coverage offered by an employer or association in which the employer takes on the risk involved with providing coverage, instead of purchasing coverage from an insurance company.
Employers or associations pay for enrollees' medical care directly, and assume the direct risk for payment of the claims for benefits.
Self-insured medical plans offer more flexibility in plan design and potential cost savings, but also carry more financial risk and administrative burden.
Self-insured medical plans are not subject to state insurance regulations and are regulated at the federal level, which means they do not have to cover services like bariatric surgery or infertility treatment, or add additional state continuation after COBRA is exhausted.
Fully-insured health plans involve employers paying a fixed premium to a health insurance carrier for their employees' medical expenses, while self-insured health plans involve employers assuming all financial risk for providing benefits to employees.