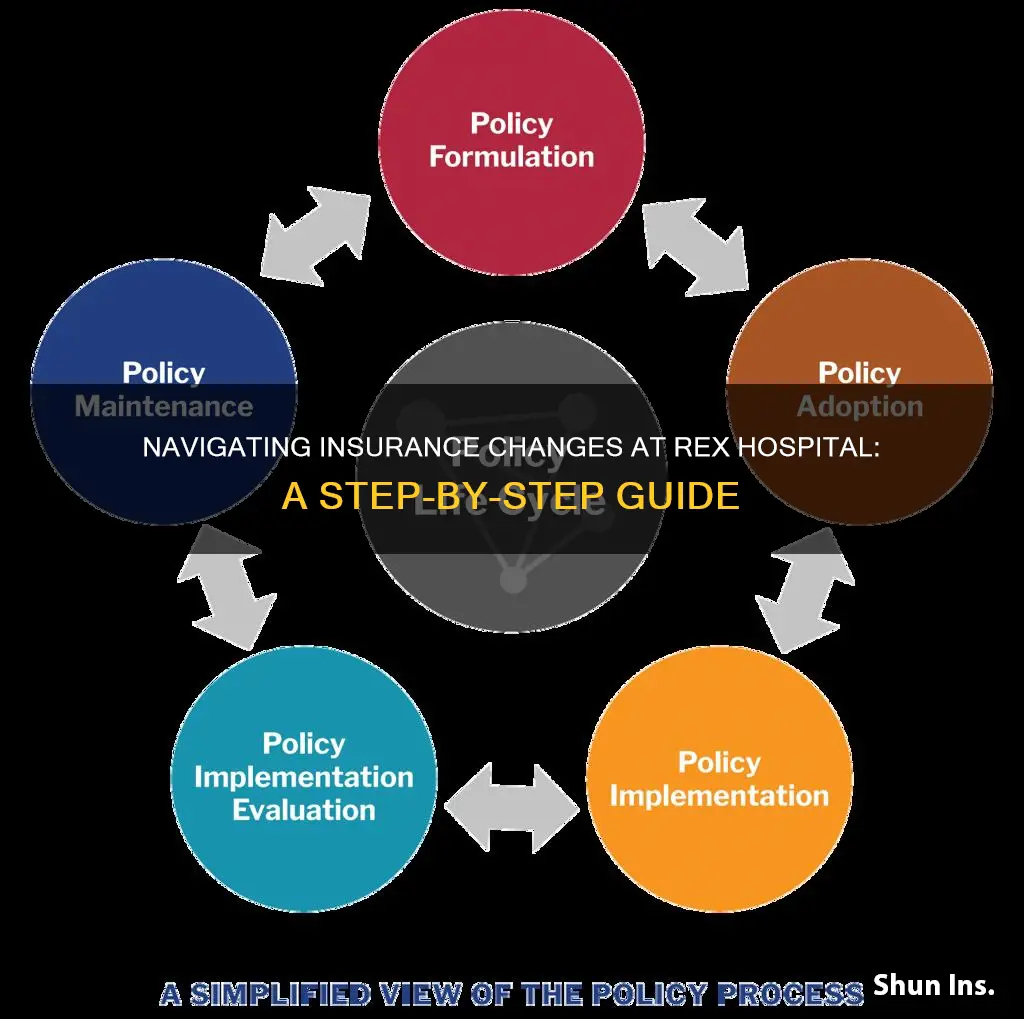
If you need to change your insurance at Rex Hospital, you can rest assured that they will assist you with obtaining the necessary approval for your visit and file your insurance claim for you. Rex Hospital accepts a variety of insurance plans, including those from UNC Lenoir Health Care, UNC Rockingham Health Care, Nash UNC Health Care, and Caldwell Memorial Hospital. To ensure that your insurance information is complete and accurate, remember to bring your insurance card and photo identification when you are admitted. You may also need to call your insurance company in advance to review your coverage and confirm any charges that may not be covered by your insurance.
| Characteristics | Values |
|---|---|
| When to call insurance company | Before your due date |
| Who will file the insurance claim | UNC REX Healthcare |
| When to add a baby to an insurance plan | After delivery |
| Who to contact for questions about registration | 919-784-3257 |
| Who to contact for questions about payment arrangements or financial assistance | (800) 594-8624 |
| Who to contact for questions about physician billing | American Anesthesiology of North Carolina, PLLC: (888) 280-9533, press #5 |
| OB Hospitalist Group: (888) 442-8454 | |
| Raleigh Radiology Associates, Inc.: (866) 788-9852 | |
| Rex Pathology Associates, PA: (919) 784-3063 |
What You'll Learn

Confirming the baby has been added to the insurance plan
Confirming that your baby has been added to your insurance plan is a crucial step in ensuring your child's health coverage. Here are some detailed steps to help you confirm this:
Contact Your Insurance Provider:
Get in touch with your insurance company as soon as possible. Most insurance companies require newborns to be added to an existing policy within 30 to 60 days of birth. You can reach out to your insurance company by using their mobile app or calling their customer service line.
Provide Necessary Documentation:
Make sure to have all the required documents ready. This typically includes your baby's birth certificate, proof of birth, hospital records, and other relevant information. The hospital where you gave birth can assist you in obtaining and submitting these forms.
Complete the Enrollment Form:
Your insurance provider will provide you with an enrollment form for your baby. Fill out this form and submit it within the required timeframe, which is usually no later than 12 months after your baby's date of birth.
Follow Up on the Status:
After submitting the enrollment form, stay in touch with your insurance company. If you don't hear back within one to two weeks, contact them directly to confirm the status of your application and ensure that your baby has been successfully added to your insurance plan.
Understand the Special Enrollment Period:
Keep in mind that having a baby is considered a qualifying life event, triggering a special enrollment period. This means you can enroll your baby in health care coverage within 30 to 60 days of their birth, and the coverage will be retroactive to their date of birth.
Explore Coverage Options:
If you have existing health insurance, you can add your baby to that plan or switch to a family plan. Compare different plans, considering factors such as premium costs, copays, covered doctors, hospitals, and medications.
Check for Confirmation:
Once you have provided all the necessary documentation and completed the enrollment process, your insurance company should confirm the successful enrollment of your baby. This confirmation can come in the form of an email, letter, or phone call.
By following these steps, you can ensure that your baby has been added to your insurance plan, providing them with the health coverage they need from the very beginning of their life.
The Evolution of Term Insurance: A Historical Perspective
You may want to see also

Registering the baby to the mother's insurance
Before the birth
It is important to be prepared when it comes to insurance for your newborn. While there is a short buffer period where the newborn will be covered under the mother's insurance, it is best to have a plan in place to avoid any gaps in coverage. Before the baby is born, review your current insurance plan and compare it with other alternatives. Consider premium costs, copays, and whether the doctors, hospitals, and medications you want are covered in each plan. If you have insurance through your employer, speak to your HR department about the options for adding a newborn to your plan.
After the birth
After the baby is born, you will need to register them to your insurance plan. The birth of a child is considered a qualifying life event that triggers a special enrollment period, allowing you to make changes to your health insurance plan outside of the regular open enrollment period. You will have a window of 30 to 60 days after the birth of your child to add them to your insurance plan. During this time, you can also switch to a different plan if you find one that better suits your new family situation.
Paperwork
To register your baby to your insurance plan, you will need to gather the necessary paperwork. Contact your insurance company to check what documents are required, as this may differ depending on the type of insurance and the company. Typically, you will need your baby's birth certificate or proof of birth. The hospital where you gave birth can help you complete and submit these forms, but it usually takes a couple of weeks to obtain them.
Costs
Adding a newborn to your insurance plan may result in increased premiums. Take the time to review your expenses and prepare for any cost changes. Family plans may allow for new dependents at no additional charge, but sometimes premiums can increase significantly.
Timeline
For the first 30 days of the newborn's life, they will be covered as an extension of the mother under her policy and deductible. Starting on day 31, the baby will need to be added to the mother's insurance plan or have their own policy.
Other Options
If you are unable to add your baby to your current insurance plan or are uninsured, you may want to consider a child-only health insurance plan. Government programs like Medicaid and the Children's Health Insurance Program (CHIP) offer free or low-cost health coverage for children from low-income families.
Billing Insurance for Wigs: A Comprehensive Guide for Medical Professionals
You may want to see also

Bringing insurance card and photo ID
To change your insurance at Rex Hospital, it is important to bring your insurance card and photo ID. This is to ensure that the hospital has complete and accurate insurance information. It is also helpful to bring these documents when pre-registering for delivery at the Women's Center.
Bringing your insurance card ensures that the hospital can accurately file your insurance claim. Rex Hospital can file primary and most secondary insurance claims when provided with complete and accurate information at the time of registration. This means that the hospital will be able to communicate with your insurance company and help you obtain the necessary approval for your visit.
Having your insurance card on hand also helps to streamline the billing process. Rex Hospital will request payment of your estimated amount due during your stay, which may include co-pay, co-insurance, deductible, self-pay amounts, or related deposits. By providing your insurance information, you can better understand what costs will be covered by your insurance plan.
Additionally, bringing your photo ID verifies your identity and helps ensure that your insurance information is correctly associated with you. This is particularly important if you have recently updated your insurance or made any changes to your personal information.
It is always a good idea to call your insurance company ahead of time to review your coverage and understand what costs may be covered by your plan. This can help you avoid unexpected expenses and provide peace of mind during your stay at Rex Hospital.
The Costly Consequences of Inaccurate Insurance Billing
You may want to see also

Calling the insurance company to review maternity coverage
Understanding Your Coverage
Before calling your insurance company, it's essential to gather information about your current plan. Review your insurance policy documents, including the fine print, to understand the specifics of your coverage. Pay close attention to the following:
- Network of providers: Identify the medical professionals and facilities that are within your insurance plan's network. This includes not only your OB-GYN and hospital but also anesthesiologists, nurses, and labs involved in your care. Staying in-network typically results in lower costs.
- Covered services: Determine what maternity and prenatal services are covered by your insurance plan. This includes prenatal visits, health screenings, lab work, ultrasounds, birthing classes, treatment for pregnancy-related medical conditions, and procedures resulting from complications.
- Coverage limits and deductibles: Check for any annual reimbursement limits or out-of-pocket maximums. Understand your deductible, which is the amount you need to pay before your insurance coverage kicks in.
- Pre-authorization requirements: Note any pre-authorization rules specified by your insurer. Some plans require pre-authorization for specific services or procedures, and failing to obtain pre-authorization may result in financial penalties.
Contacting the Insurance Company
Once you have a good understanding of your policy, it's time to call your insurance company. Here are some key questions to ask and points to discuss:
- Confirm coverage: Verify that your plan covers maternity and prenatal care. Although it is mandated by the Affordable Care Act, it's always good to double-check.
- In-network providers: Ask for a directory of in-network providers, including obstetricians, hospitals, and other specialists. Staying within this network will help minimize out-of-pocket expenses.
- Pre-authorization requirements: Confirm if pre-authorization is needed for any specific maternity or prenatal services. For example, some plans require pre-authorization for ultrasounds or amniocentesis.
- Coverage for complications: Discuss coverage for potential pregnancy complications. Understand how your plan covers procedures or treatments resulting from complications, unplanned obstetrical surgery, epidurals, premature births, or extended stays in the neonatal unit.
- Coverage for newborn: Inquire about coverage for your newborn. Ask about the procedure for adding your baby to your plan and the timeframe for doing so. Understand the coverage provided for well-child care, pediatric visits, immunizations, and vaccinations.
- Referrals and specialists: Clarify if you need a referral from your primary care physician to see an obstetrician or specialist. Some plans may require this, especially in the event of complications.
- Coverage limits and deductibles: Discuss any annual reimbursement limits and confirm if there is an out-of-pocket maximum. Understand how your deductible applies to maternity and prenatal care.
- Alternative birthing options: If you are considering a birth center or home birth, ask about coverage for these options. Some plans may have specific requirements or limitations for out-of-hospital births.
Additional Considerations
While reviewing your maternity coverage, keep the following in mind:
- Compare plans: If you have the option to switch insurance plans, compare different policies to find one that best suits your needs. Consider factors such as network size, covered services, deductibles, and customer satisfaction.
- Understand your deductible: Know your deductible amount and how it applies to maternity care. Remember that the full cost of pregnancy and delivery will likely exceed your deductible, so be prepared to pay the full deductible amount.
- Take advantage of resources: Many insurance companies offer resources and programs specifically designed for pregnant women. These may include access to nurses, prenatal care information, parenting classes, or support groups.
- Explore lower-cost options: If you're uninsured or underinsured, explore lower-cost options such as Medicaid, the Children's Health Insurance Program (CHIP), community health centers, or charitable organizations that provide maternity care.
Switching Insurance: Exploring Options for Retaining Preferred Doctors
You may want to see also

Filing primary and secondary insurance claims
Understanding Primary and Secondary Insurance
Firstly, it is important to understand the difference between primary and secondary insurance. The primary insurance policy is the policy that claims will be billed to first. The secondary insurance payer will then cover a portion of the remaining balance, which often includes the patient's copay. Typically, a patient's coverage from their employer will be primary insurance, and their coverage from a spouse or parent will be secondary insurance.
Identifying Primary and Secondary Insurance
To identify which insurance is primary and which is secondary, you should ask the patient to designate their preferred primary and secondary insurance using a coordination of benefits form. In the case of minors and young adults covered under their parent's insurance plans, the birthday rule determines which plan is primary and which is secondary. The parent whose birthday falls first in the year will have the primary insurance plan.
Filing Claims
When filing insurance claims, the primary claim is sent before the secondary claim. Once the primary payer has paid their portion of the bill, you will be able to send the claim to the secondary payer. It is important to note that you cannot submit a claim to both insurance companies at the same time. After the primary insurance claim has been processed, submit the claim to the secondary insurance company, including the total that was billed initially, how much the primary insurer paid, and why the primary insurer didn't pay the full balance.
Common Issues
One common issue with secondary insurance claims is rejection due to missing or invalid information. This usually means that the total billed amount of the secondary claim does not balance with the primary payment amount and claim adjustments. To avoid this, ensure that you communicate the reasons why the billed amount was not paid in full by the primary insurer. Another common issue is related to coordination of benefits, which can be time-consuming to resolve.
Unraveling the Mystery of List Bills in Insurance: A Comprehensive Guide
You may want to see also
Frequently asked questions
You can update your insurance information by bringing your insurance card and photo identification to the hospital when you are admitted.
After delivery, you must add your baby to your insurance plan. Rex Hospital will register the baby to the mother's insurance. If you want to register your baby to a different insurance plan, you can change this after confirming with that insurance plan.
UNC REX Healthcare will assist you with filing your insurance claim. They can file primary and most secondary insurance claims when provided with complete and accurate information at the time of registration.