An insurance billing worksheet is a document that helps patients understand their medical bills. Medical billing in the United States can be a complex process, with many patients confused by their medical bills. An insurance billing worksheet provides a breakdown of the services provided, the corresponding charges, and the amounts covered by insurance. It is important for patients to review their insurance billing worksheets carefully to identify any billing errors and ensure they are not overcharged for medical services.
What You'll Learn

Medical coding
The process of medical coding starts when a patient visits a physician's office, hospital, or other healthcare facility. During the patient encounter, providers detail the visit or service in the patient's medical record, explaining the reasons for delivering specific services, items, or procedures. Accurate and complete clinical documentation during the patient encounter is critical for medical billing and coding. The golden rule in this field is, "Do not code it or bill for it if it's not documented in the medical record."
Once the patient leaves the healthcare facility, a professional medical coder reviews and analyses the clinical documentation. They connect the services provided with billing codes related to the diagnosis, procedure, charge, and professional and/or facility code. Coders use various code sets during this process, including ICD-10 diagnosis codes, CPT and HCPCS procedure codes, charge capture codes, and professional and facility codes.
Diagnosis codes, such as the ICD-10 codes, are essential for describing a patient's condition or injury, as well as social determinants of health. On the other hand, procedure codes, like CPT and HCPCS, indicate what procedures or services were performed during the patient encounter. These codes are then used by medical billers to create insurance claims and patient bills, forming the backbone of the healthcare revenue cycle.
The medical coding process can be complex and time-consuming, depending on the complexity of the services rendered and the organisation's claim denial management. It requires a strong understanding of medical terminology and coding guidelines to ensure accurate reimbursement and avoid billing errors.
The Intricacies of COB Insurance Clauses: Unraveling Coordination of Benefits
You may want to see also

Medical billing
Front-End Medical Billing
The front-end medical billing process begins when a patient registers at a healthcare facility and schedules an appointment. During pre-registration, administrative staff ensure that patients complete the necessary forms and confirm their personal and insurance information. The staff also verify if the patient's health plan covers the requested services and confirm the patient's financial responsibility. During this process, patients are informed about any costs they are responsible for, and co-payments are collected if possible.
Medical Coding
Once the patient checks out, medical coders obtain the medical records and translate them into standardised codes. This process involves extracting billable information from the medical record and clinical documentation. Accurate and complete clinical documentation is critical for medical billing and coding. The codes are then used to create insurance claims and bills for patients.
Back-End Medical Billing
In the back-end medical billing process, medical coders and billers work together to create a "superbill". This is an itemised form that includes provider information, patient information, and visit information such as procedure codes, diagnosis codes, and service dates. Billers then prepare and submit claims to insurance companies, either directly or through a third-party organisation.
Adjudication and Payment
Once the insurance company receives the claim, they assess the provider's claim and determine the reimbursement amount. This process is called adjudication, and the insurance company can accept, deny, or reject the claim. After adjudication, the insurance company sends an Explanation of Benefits (EOB) to the patient, explaining what they paid for and why. The insurance company then reimburses the healthcare provider, and the patient receives a bill for any remaining balance.
Understanding the Insured's Road to Restoration: A Guide to Insurance Restoration
You may want to see also

Explanation of Benefits (EOB)
An Explanation of Benefits (EOB) is a document sent to insured individuals by their insurance company after a claim has been submitted by a healthcare provider. It is not a bill, but it does show a balance due. An EOB is a valuable tool for consumers to keep informed of their healthcare costs and expenditures. It also offers insured customers a chance to double-check that services are billed correctly.
An EOB will show the insured individual:
- The services they received and the date they received them
- The amount the healthcare provider is charging the insurance company
- The amount the insurance company has paid the healthcare provider
- The amount the insurance company has not covered
- The amount the insured individual is responsible for paying
- The amount the insured individual has already paid
- The amount the insured individual may owe the healthcare provider
- The amount the insured individual may owe the insurance company
- Any money saved by visiting in-network providers
- Any out-of-pocket medical expenses the insured individual will be responsible for
- Any deductible, copay, or coinsurance amount
- The total amount the insurance company has paid to the healthcare provider
- The total amount the insured individual owes the healthcare provider
It is important to keep EOBs organized, for example, by filing them by date. This way, they can be easily accessed should questions arise.
A Comprehensive Guide to Insurance Billing with Office Ally
You may want to see also

Pre-registration
During pre-registration, administrative staff ensure that patients complete the required forms and confirm patient information, including home address and insurance coverage. They also verify that the patient's health plan will cover the requested services and submit any prior authorizations. This helps to improve patient flow and reduce wait times.
Items typically required for pre-registration include:
- Insurance card and driver's license
- The name of the doctor who ordered the procedure
- The date of the appointment
- Emergency contact information
Healing Arts: Navigating Insurance Billing for Reiki Practices
You may want to see also

Deductibles
A health insurance deductible is the amount an individual or family pays out-of-pocket for healthcare services before their insurance coverage begins to share the costs. Deductibles are typically annual and must be met before insurance benefits will subsidise payment. Deductibles vary depending on the insurance plan and the number of people covered.
For example, if an individual has an insurance plan with a $2,500 deductible, they must pay $2,500 in qualifying payments before the insurance pays for any services. Until the deductible is met, the individual is responsible for paying 100% of the services covered by the insurance plan. Once the deductible has been met, the insurance will kick in and begin sharing the cost of covered services. At this point, the individual will pay a copayment or coinsurance for all services covered by the plan, and the insurance company will pay for the rest.
The average individual yearly deductible was $5,101 during the Open Enrollment Period in 2024, while families had an average deductible of $10,310.
There are two main types of deductibles: individual and family. An individual deductible applies to individual health insurance plans, covering one person. A family deductible applies to family health insurance plans, covering multiple people.
In addition, there are high-deductible health plans (HDHPs) and low-deductible health plans. HDHPs have higher deductibles but lower monthly premiums, while low-deductible plans have lower deductibles and higher monthly premiums. As a result, HDHPs offer more significant cost-sharing responsibilities to insured individuals, whereas low-deductible plans offer more generous coverage of medical services.
When choosing between a high-deductible or low-deductible plan, individuals should consider their health needs, budget, and risk tolerance. Those who are generally healthy and don't require frequent medical care may prefer a high-deductible plan with lower monthly costs. On the other hand, those who anticipate higher medical expenses or want more comprehensive coverage may opt for a low-deductible plan, despite the higher monthly premiums.
Understanding Insurance Billing for Lactation Services: A Guide for Healthcare Providers
You may want to see also
Frequently asked questions
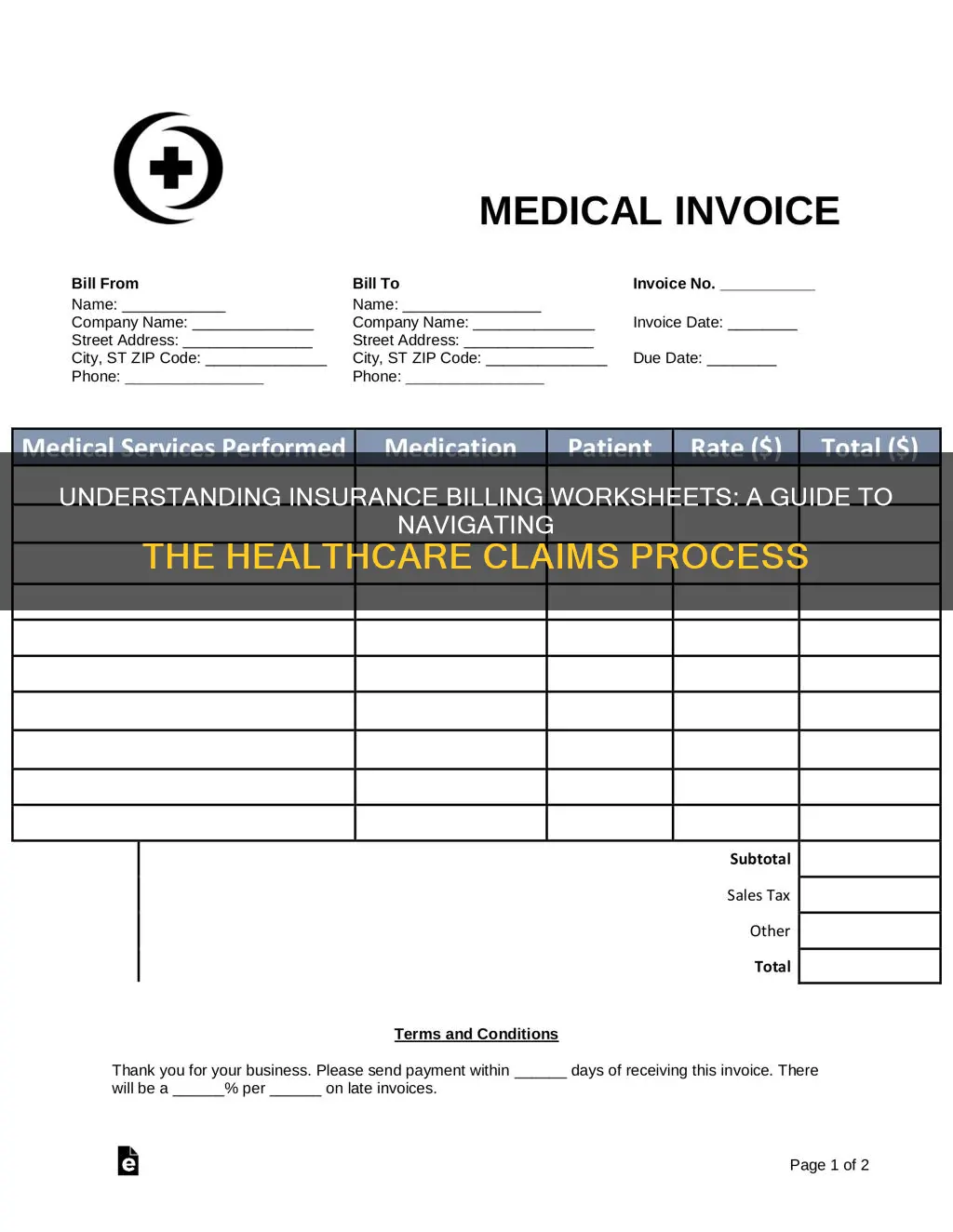
An insurance billing worksheet is a document that details the costs of medical services provided to a patient. It includes information such as the date of service, the type of service provided, and the corresponding charges.
An insurance billing worksheet is not the same as a bill. It is a document that outlines the costs of medical services provided, while a bill is a printed summary of the amount owed by the patient or their insurance company for those services.
An insurance billing worksheet typically includes the following information:
- Date of service
- Description of service
- Charges for each service
- Total amount owed
- Insurance coverage information
An insurance billing worksheet is usually created by the healthcare provider, such as a hospital or physician's office. They use the worksheet to bill the patient or their insurance company for the services provided.