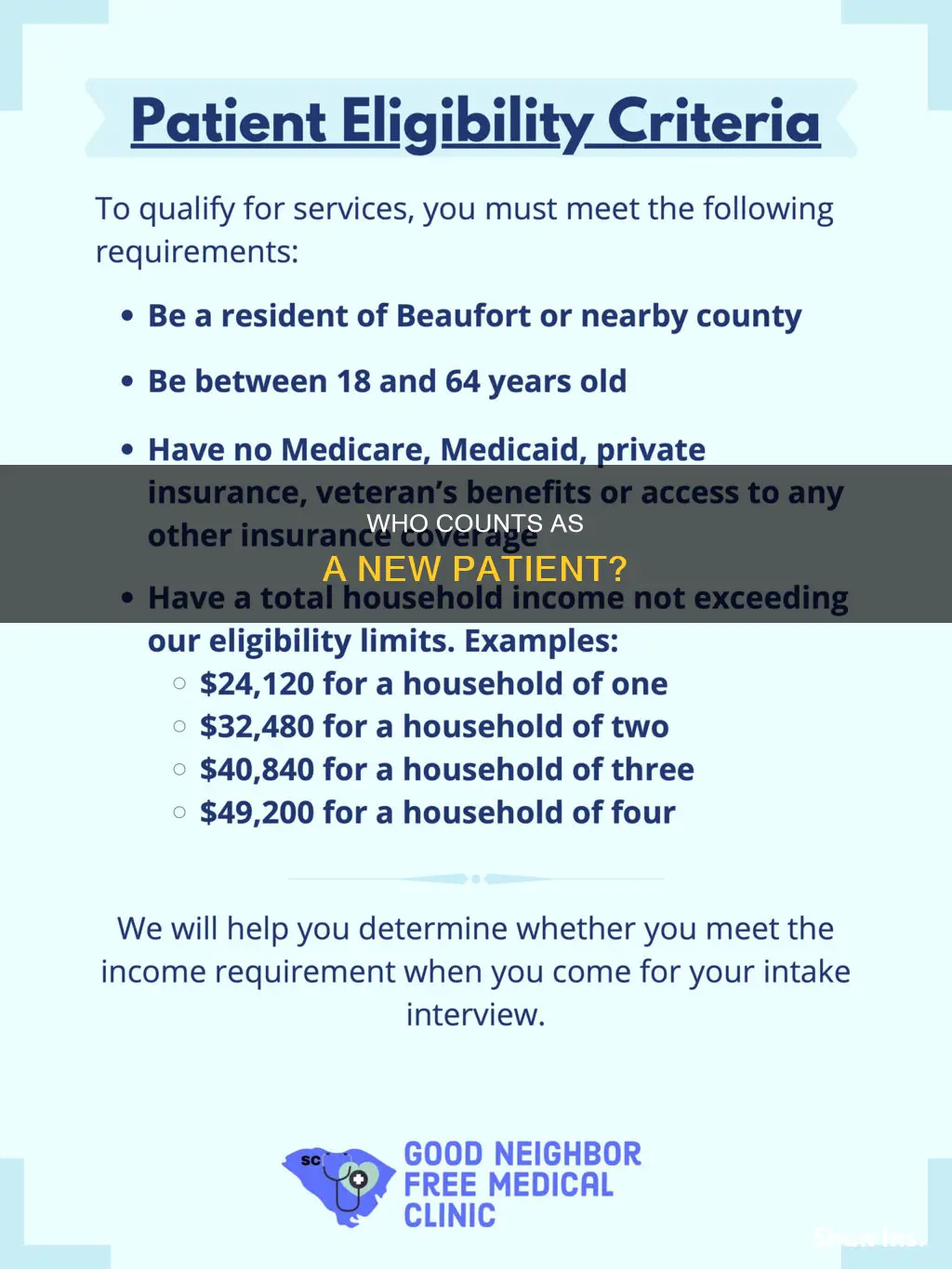
Whether a patient is considered a new patient for insurance purposes depends on a few factors. According to the CPT code book, a new patient is someone who has not received any professional services from a physician or qualified healthcare professional of the same specialty and subspecialty within the same group practice in the past three years. This three-year rule is a general guideline and some payers may have different criteria. The location of service does not change a patient's status, nor does a change in tax ID or physical location. Additionally, an interpretation of a diagnostic test, such as reading an X-ray or EKG, does not affect the designation of a new patient if it is done in the absence of a face-to-face service.
| Characteristics | Values |
|---|---|
| Time since last visit | A patient is considered new if they have not been seen by a physician or another physician or other qualified health care professional of the same specialty in the same group practice in the past three years. |
| Face-to-face service | "Seen" means for a face-to-face service. An interpretation of a diagnostic test, reading an X-ray or EKG etc., in the absence of a face-to-face service with the patient does not affect the designation of a new patient. |
| Location of service | Where the patient was seen doesn't matter. If a physician cares for a patient in the hospital and then provides follow-up service in the office, the patient is established to the physician, even if it is the first time the patient presents to the office. |
| Physician's group practice | A patient is considered new if they have not received any professional services from the physician group practice (same physician specialty) within the previous 3 years. |
| Specialty | A patient is considered new if they have not received any professional services from another physician or other qualified health care professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years. |
What You'll Learn
- A new patient is one who hasn't received professional services from a physician or qualified healthcare professional in the same group practice within the past three years
- The three-year rule: A previous, face-to-face service must have occurred at least three years from the date of service to be considered a new patient
- Different specialty/subspecialty within the same group: This area causes confusion as doctors switching practices can complicate whether a patient is new or established
- Interpretation of a diagnostic test: An interpretation of an X-ray or EKG, without an E/M service or face-to-face meeting, does not affect the designation of a new patient
- Professional service: Face-to-face services rendered by a physician and reported by a specific CPT code

A new patient is one who hasn't received professional services from a physician or qualified healthcare professional in the same group practice within the past three years
When it comes to insurance, determining whether an individual is a new patient or an established patient is crucial for billing purposes. The distinction between a new and established patient hinges on the timeframe since the patient last received professional services from a physician or qualified healthcare professional.
A new patient, according to the CPT® code book, is defined as:
> "A new patient is one who has not received any professional services from the physician/qualified healthcare professional or another physician/qualified healthcare professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years."
In simpler terms, if an individual has not had any face-to-face services or professional interactions with a physician or qualified healthcare professional within the same group practice in the last three years, they are considered a new patient for insurance purposes. This definition is further clarified by the Centers for Medicare & Medicaid Services (CMS) in the Medicare Claims Processing Manual, which specifies that interpretations of diagnostic tests, such as reading an X-ray or EKG, do not affect the designation of a new patient if they are done in the absence of a face-to-face service.
The three key components that define a new patient are:
- Professional Service: This typically refers to face-to-face services provided by a physician or qualified healthcare professional. If a provider has only billed for radiology or lab tests without a face-to-face encounter, a new patient code should be billed when the patient is seen for the first time.
- Three-Year Rule: The general guideline is that a patient is considered new if they have not had a previous, face-to-face service within the last three years from the date of service. Some payers may use slightly different guidelines, such as considering the month of the previous visit instead of the exact day.
- Different Specialty/Subspecialty within the Same Group: This area can be confusing, but it refers to situations where a patient sees a different specialist within the same group practice. If the specialists have different taxonomy codes, they may be considered separate specialties, and a new patient code could be billed.
It is important to note that this definition of a new patient applies specifically to billing and insurance contexts and may not align with common sense interpretations of whether a patient is "new." Additionally, not all E/M (Evaluation and Management) codes differentiate between new and established patients. For example, in an emergency department (ED), the patient is always considered new, and the provider is expected to document the patient's history in the medical record.
Understanding Insurance Billing for Partial Denture Procedures: Timing and Coverage
You may want to see also

The three-year rule: A previous, face-to-face service must have occurred at least three years from the date of service to be considered a new patient
The three-year rule is a key factor in determining whether a patient is considered 'new' or 'established' for insurance purposes. This rule states that a patient is considered 'new' if they have not received any professional services or face-to-face encounters from a physician or qualified healthcare professional of the same specialty and subspecialty within the same group practice in the past three years.
This rule is important for billing and insurance reimbursement purposes, as new patient codes carry higher relative value units (RVUs) and are, therefore, scrutinised closely by payers. The three-year rule helps to ensure accurate billing and reimbursement, reducing the risk of fraudulent claims or denials.
The three-year rule is applied when a patient has had a previous, face-to-face service with a physician or healthcare professional. This service could include an evaluation and management (E/M) service, surgical procedure, or other face-to-face encounter. The date of this previous service is compared to the date of the current service to determine if three years have passed. If the previous service occurred at least three years ago, the patient is considered 'new' for the current service.
It is important to note that the three-year rule applies regardless of changes in tax ID or physical location. If a patient has received services from a physician or healthcare professional within the same specialty and subspecialty group practice, they are considered 'established', even if that group practice has changed locations or tax IDs.
Additionally, the three-year rule takes precedence over the treating physician's National Provider Identifier (NPI). If a patient has seen a physician within the same specialty and subspecialty group practice, they are considered 'established' for insurance purposes, even if they are now seeing a different physician with a unique NPI within that group.
The three-year rule also applies when a patient is seen by a covering or on-call physician from a different practice. If the patient has had a previous face-to-face encounter with their regular physician within the three-year period, they are considered 'established' for the covering physician, regardless of the practice location or NPI.
In summary, the three-year rule is a critical component in determining whether a patient is 'new' or 'established' for insurance purposes. It ensures accurate billing and reimbursement by considering the timing and nature of previous face-to-face encounters with healthcare professionals of the same specialty and subspecialty within a group practice.
Understanding Door Dash Insurance: Making Changes to Suit Your Needs
You may want to see also

Different specialty/subspecialty within the same group: This area causes confusion as doctors switching practices can complicate whether a patient is new or established
The area of greatest confusion when it comes to determining whether a patient is new or established is when doctors switch practices within the same group. This is especially pertinent for Medicare patients, who can use the National Provider Identifier (NPI) registry to see what specialty the physician’s taxonomy is registered under. For other payers, this is usually determined by the way the provider was credentialed.
If a doctor changes practices and takes their patients with them, they cannot bill the patient as new based on the new tax ID. The tax ID does not matter in this case, as the provider has already seen these patients and established a history.
If a doctor of medicine (MD) or doctor of osteopathy sends a patient to a mid-level provider (e.g. a nurse practitioner or physician assistant) and the visit does not fall under incident-to, the mid-level provider should calculate whether the patient is new or established based on the specialty they are working in. If the MD is a family practice provider and the nurse practitioner sees hematology patients, for example, the specialty is different and a new patient code can be billed. However, if the nurse practitioner is also considered family practice, it would not be appropriate to bill a new patient code.
If one provider is covering for another, the covering provider must bill the same code category that the regular provider would have billed, even if they are a different specialty. For example, if a patient’s regular physician is on vacation, and the patient sees a covering physician from a different specialty, the covering physician must still bill an established patient code.
Insurance Policy Changes: Navigating the Cost Conundrum
You may want to see also

Interpretation of a diagnostic test: An interpretation of an X-ray or EKG, without an E/M service or face-to-face meeting, does not affect the designation of a new patient
When determining whether a patient is new or established, it is important to refer to the CPT code book. According to CPT, a new patient is one who has not received any professional services, i.e., an E/M service or face-to-face service (e.g., a surgical procedure) from the physician or physician group practice (same physician specialty) within the previous 3 years. This means that if a patient has received any professional services, E/M service, or a face-to-face service from the provider or another provider of the same specialty in the same group practice within the previous three years, they are considered an established patient.
An interpretation of a diagnostic test, such as reading an X-ray or EKG, does not affect the designation of a new patient if it is done in the absence of an E/M service or other face-to-face service with the patient. This means that if the only interaction between the patient and the physician is the interpretation of an X-ray or EKG, without any additional E/M service or face-to-face meeting, then the patient is still considered a new patient.
For example, if a patient presents to the emergency department with chest pain and the ED physician orders an electrocardiogram (EKG) which is interpreted by the cardiologist on call, the cardiologist would bill for the EKG interpretation. If the patient is then sent home and asked to follow up with the cardiologist for further evaluation, the subsequent visit with the cardiologist would still be considered a new patient visit, as the only prior interaction was the interpretation of the EKG without any face-to-face service.
It is important to note that Medicare and other payers may have specific guidelines and policies regarding new patient designations and billing. Additionally, different specialties and subspecialties within the same group can also impact whether a patient is considered new or established. It is crucial to refer to the CPT code book, payer policies, and seek guidance from billing and coding experts to ensure accurate and appropriate billing practices.
Strategies for Managing a Hefty Insurance Bill
You may want to see also

Professional service: Face-to-face services rendered by a physician and reported by a specific CPT code
The Current Procedural Terminology (CPT) code system is a standardised coding system for medical services and procedures. CPT codes are used to identify and report on professional services rendered by qualified healthcare professionals (QHPs). CPT codes are five-digit numeric or alphanumeric codes, depending on the category.
CPT codes are essential for accurately capturing healthcare data and processing health claims for Medicare, Medicaid, and other health programs. The CPT code set is developed and maintained by the American Medical Association (AMA) and is the preferred system for coding and describing healthcare services and procedures in federal programs (such as Medicare and Medicaid) and throughout the United States by private insurers and providers of healthcare services.
When it comes to determining whether an individual is a new patient or an established patient, there are a few key components to consider. According to the CPT code book, a new patient is defined as:
> "A new patient is one who has not received any professional services from the physician/qualified health care professional or another physician/qualified health care professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years."
This definition is further elaborated by the Centers for Medicare & Medicaid Services (CMS) in the Medicare Claims Processing Manual, Chapter 12 – Physicians/Nonphysician Practitioners (30.6.7):
> "An interpretation of a diagnostic test, reading an X-ray or EKG etc., in the absence of an E/M service or other face-to-face service with the patient does not affect the designation of a new patient."
In other words, if a patient has not had a face-to-face service or visit with a physician or qualified healthcare professional of the same specialty within the past three years, they are considered a new patient. This three-year rule is a general guideline, and some payers may have slightly different guidelines, such as using the month of the previous visit instead of the day.
It is important to note that not all Evaluation and Management (E/M) codes fall under the new vs. established patient categories. For example, in an emergency department (ED), the patient is always considered new, and the provider is expected to document the patient's history in the medical record.
Additionally, the provider's National Provider Identifier (NPI) is used to track if the patient has been seen within the previous three years. This information can be found on the NPI website or by checking with the credentialing department or payer.
In summary, when determining whether to bill for a new or established patient, it is essential to consider the definition of a new patient as outlined in the CPT code book, the CMS guidelines, the three-year rule, the specialty of the provider, and the patient's history of face-to-face services within the same group practice.
Understanding the Term Booster: Unlocking the Full Potential of Your Insurance Policy
You may want to see also
Frequently asked questions
A new patient is one who has not received any professional services from the physician/qualified health care professional or another physician/qualified health care professional of the exact same specialty and subspecialty who belongs to the same group practice within the past three years.
No, a patient's insurance status does not affect whether they are considered a new patient.
No, if a patient has seen a physician of the same specialty at a different practice location within the same group, they are still considered an established patient.
Yes, "seen" means for a face-to-face service.
For the purpose of determining whether a patient is new or established, CPT considers physician assistants or nurse practitioners to be the same specialty as the physician they work with.