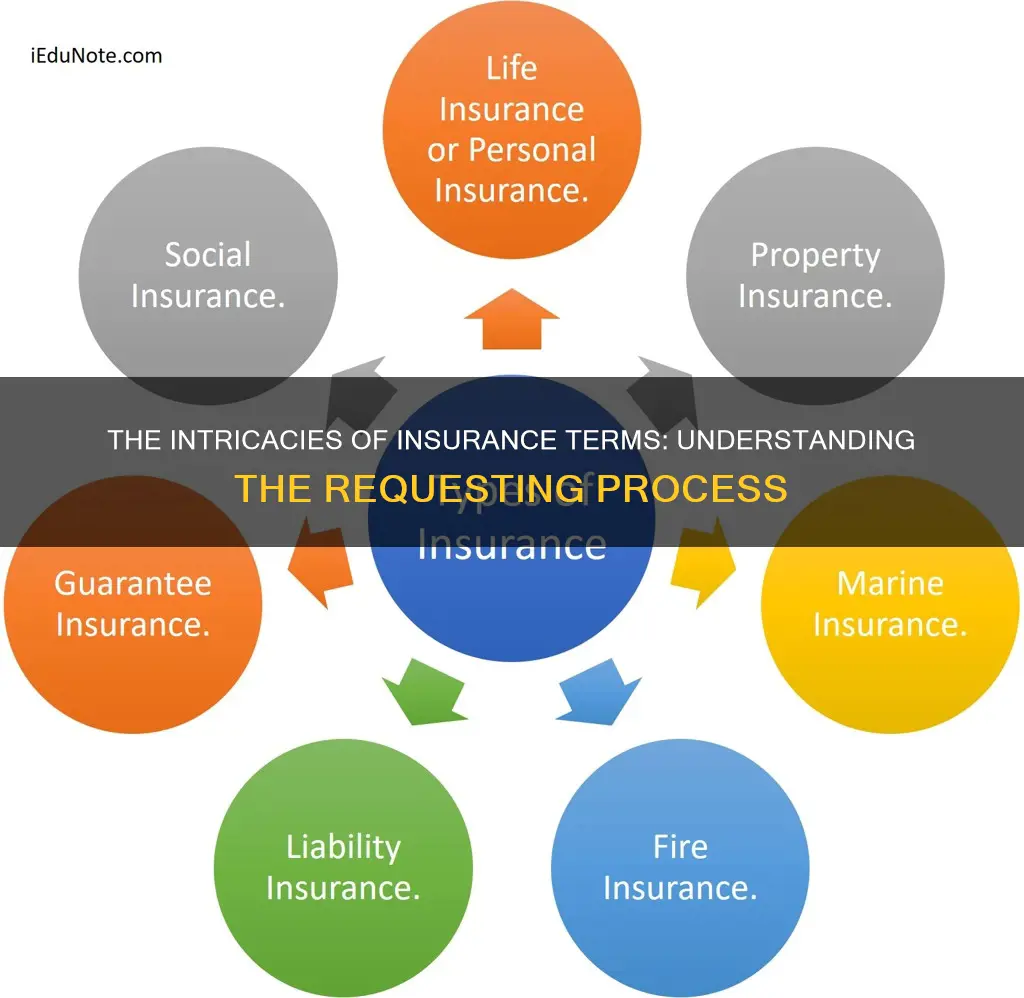
Insurance is a complex industry with its own unique language, and insurance terms can be confusing for those outside the sector. However, it is important for consumers to understand insurance jargon so they can find the right coverage for their needs. Here is a brief introduction to some of the most common insurance terms:
- Claim: A formal request by a policyholder to their insurer for compensation for a covered loss or damage.
- Claimant: The person who files the claim, usually the policyholder.
- Conditions: The section of a policy document outlining the duties and responsibilities of both the insured and the insurer, as well as the requirements for the coverage to be valid.
- Effective Date: The date when the insurance policy comes into force.
- Declarations Page: A summary of the policy details, including coverages, limits, deductibles, and the effective date.
- Deductible: The amount the policyholder agrees to pay out-of-pocket before the insurance company covers the rest.
- Hazard: A situation that increases the likelihood of a loss occurring.
- Lapse in Coverage: A period when someone goes without insurance coverage.
- Loss: The basis for filing an insurance claim, including direct and accidental damage sustained by the insured or their property.
- Named Insured: The person or business named in the policy, also known as the policyholder.
- Peril: Something that causes a loss, such as fire, theft, collisions, natural disasters, illnesses, or death.
- Policy: A written contract between the policyholder and the insurer outlining the details of the coverage.
- Premium: The amount charged by an insurance company for coverage, influenced by factors such as age, gender, driving history, and medical history.
- Rider: An optional coverage that policyholders can add to their policies, such as identity theft or roadside assistance.
| Characteristics | Values |
|---|---|
| Claim | A formal request made by the insured to the insurer for compensation for a covered loss or policy event |
| Claimant | The person who files the claim. Usually the policyholder |
| Conditions | The section of a policy document that explains the duties and responsibilities of the insured and the insurance company |
| Commencement Date | The date when the insurance policy goes into force |
| Coverage | The actual protection provided by the insurance company |
| Deductible | The amount the policyholder agrees to pay out-of-pocket before the insurance company shoulders the cost |
| Hazard | A situation or condition that raises the likelihood of a loss |
| Insured | The person or business named in the policy, also referred to as the policyholder |
| Lapses | A period when one goes without insurance coverage |
| Loss | The basis for filing an insurance claim |
| Perils | Something that causes a loss |
| Policy | A written contract between the policyholder and the insurer that lays out the details of the coverage |
| Premium | The amount charged by an insurance company in return for coverage |
| Rider | An optional coverage that policyholders can add to their policies |
What You'll Learn

Deductibles and premiums
When it comes to insurance, there are two key terms that are important to understand: deductibles and premiums.
A premium is a recurring payment made to an insurance company to purchase a specific amount of insurance coverage. It is typically paid monthly, quarterly, half-yearly, or annually during the premium payment term of the insurance policy. The premium amount is determined based on various factors such as age, health, and medical history. The higher the sum assured, the lower the premium. Premiums are usually paid to keep a health care plan active and can be covered by an employer for those with an employer-sponsored plan.
A deductible is the amount of money one must pay out-of-pocket for covered health care expenses before their insurance company begins to pay. In other words, it is the amount of money you need to spend on your health care each year before your health insurance kicks in. Certain services, such as preventive care like annual check-ups, are often provided through your health plan without additional costs and do not count towards meeting your deductible. The deductible amount varies by plan, but covered office visits and prescription drugs usually count towards it. There is no penalty if you don't meet your deductible in a given year.
The relationship between deductibles and premiums is such that plans with lower monthly premiums typically have higher deductibles, while plans with higher monthly premiums tend to have lower deductibles. Lower deductibles mean that you will pay more each month, but your insurance plan will start sharing the costs sooner. On the other hand, higher deductibles result in lower monthly premiums, but you will need to pay more upfront when you need care. This can make your expenses less predictable.
When choosing an insurance plan, it is important to consider both the premium and deductible amounts, as well as your expected health care needs and financial situation. If you anticipate frequent doctor visits or regular prescriptions, a plan with a higher premium and lower deductible may be more suitable. On the other hand, if you are relatively healthy and only expect to use preventive care, a plan with a lower premium and higher deductible may be a more cost-effective option.
The Pitfalls of Pit Carrier Insurance: Understanding the Unique Challenges
You may want to see also

Claimants and claims
A claimant is the person who files an insurance claim. In most cases, this is the policyholder. A claim is a formal request made by the insured to the insurer for compensation for a covered loss or policy event. The process for filing a claim should be smooth and efficient.
The adjuster must determine the cause of loss, whether the loss is covered by the policy, the value of the loss, and the amount of loss payable by the policy. After the evaluation, the adjuster will calculate the insurance company's potential liability to the insured and negotiate to settle the case.
The policyholder is responsible for paying the deductible, which is the amount of money paid by the insured in a claim before the insurance company covers the rest. The higher the deductible, the lower the premium, and vice versa.
The policy document will outline the duties and responsibilities of both the insured and the insurer, as well as the requirements that need to be met for the coverage to be valid. It will also include the effective date, which is when the insurance policy goes into force.
The declarations page, often located on the front page of the policy, summarises the details of the policy, including coverages, limits, deductibles, and the effective date. It is recommended that all the information on this document be carefully reviewed for correctness.
Understanding the Nature of Prepaid Insurance: A Short-Term Asset Strategy
You may want to see also

Liability coverage
Bodily injury liability helps pay for the other driver's medical bills, lost income, and emergency aid if they're hurt in a car accident and you're at fault. Property damage liability helps pay for repairs if you damage someone else's property, like their fence or car.
The amount your insurer will pay for a covered liability insurance claim depends on the coverage limits you choose. Each state sets minimum coverage limits for bodily injury liability and property damage liability that drivers must purchase, but you may decide to buy additional coverage.
Liability insurance is also called third-party insurance because it pays third parties, and not policyholders. It's critical for those who are liable and at fault for injuries sustained by other people or in the event that the insured party damages someone else's property. Liability insurance policies cover any legal costs and payouts an insured party is responsible for if they are found legally liable. Intentional damage and contractual liabilities are generally not covered in liability insurance policies.
Personal liability, workers' compensation, and commercial liability are types of liability insurance. Liability insurance can also be purchased by business owners and is typically called "general liability insurance". It's designed to protect businesses from claims related to others' bodily injury, property damage, and more.
Term Insurance Payout Frequency: Unraveling the Mystery of When Benefits Are Disbursed
You may want to see also

Insurance adjusters
An insurance adjuster, also known as a claims adjuster, is a person who investigates an insurance claim to determine whether the insurer should pay for damage or injuries, and if so, how much they should pay. They handle any kind of claim, from property damage to personal injury claims.
Claims adjusters have three main priorities: preventing insurance fraud, settling claims quickly, and settling claims for a low amount. They inspect property damage or personal injury claims to determine how much the insurance company should pay for the loss. They might inspect a home, a business, or an automobile. They interview the claimant and witnesses, inspect the property, and do additional research, such as looking at police reports. They may consult with other workers, such as accountants, architects, construction workers, engineers, lawyers, and physicians, who can offer a more expert evaluation of a claim.
Adjusters gather information—including photographs and statements, either written or recorded—and put together a report for claims examiners to review. When the examiner approves the claim, the adjuster negotiates with the policyholder and settles the claim. If the claimant contests the outcome of the claim or the settlement, adjusters work with attorneys and expert witnesses to defend the insurer’s position.
There are three types of insurance claims adjusters: staff adjusters, independent adjusters, and public adjusters. Staff adjusters work full-time for a single insurance company and are typically salaried employees. Independent adjusters are self-employed contractors who work with multiple insurance companies, often travelling to areas after a major weather event or emergency. Public adjusters work for the policyholder, helping people and business owners to file an insurance claim if the proposed settlement seems unfit.
To become a claims adjuster, you will typically need a high school diploma or equivalent, although some positions require a bachelor’s degree or insurance-related work experience. Many states require claims adjusters to be licensed, which involves taking a course and passing a licensing exam.
Unveiling the VM Insurance Term: Understanding Virtual Management Coverage
You may want to see also

Insurance contract termination
Reasons for Termination
There are a variety of reasons why someone may want to terminate their insurance contract. For example, the insurance company may be failing to reimburse according to contract provisions, or they are spending too much time chasing reimbursement. Other reasons could be additional costs, excessive administrative expectations, or the contract is not supporting the practice with a steady flow of clients or competitive rates.
Planning for Termination
Before terminating your insurance contract, it is important to do some financial planning. First, determine how much income you could lose by terminating the contract. To do this, count how many weekly clients you have using that payer, multiply that by the contracted rate, and then multiply that number by four weeks. This will give you the maximum amount of money you could lose in your first month without that insurance. It is unlikely that you will lose all your clients from that payer, especially if you are willing to provide documentation for out-of-network benefits.
Next, figure out how many full-fee clients you will need to add to make up for the loss. You may also need to plan for any changes in your budget, such as ramping up your caseload for a few months or cutting back on spending.
Notifying Clients
It is important to give your clients plenty of notice when you are terminating your insurance contract. Letting clients know at least a few months in advance can reduce their stress and yours, significantly. Provide clients with written and verbal notice. During a session, talk with the client and let them know that a form will need their signature and will be sent through the patient portal. In the letter, include information about their options, such as using out-of-network insurance benefits or reimbursement through a health savings account.
Terminating the Contract
Look ahead at the date you would like to have your contract terminated and plan for any extra time you will need to help clients through transitions, such as discharges or referrals. Write a letter to the payer stating your intention to terminate the contract and send it to the contract's administrator or the person specified in the contract for contract-related issues. Send the letter by certified mail with a return receipt requested so there is no ambiguity about whether the payer received the letter. Follow up with a phone call or email to ensure they received your letter.
Legal Requirements
The legal requirements for terminating an insurance contract vary depending on the country and type of insurance. In general, both parties to the contract (the policyholder and the insurer) are free to determine the term of the insurance contract. The notice period for termination must be equal for both parties and is typically between one and three months. An insurance contract entered for an indefinite period may normally be terminated by either party before the end of the current insurance period. For insurance contracts concluded for a term of more than three years, the policyholder often has a special right of termination from the end of the third insurance year.
The Renewal Riddle: Unraveling the Mystery of Level Term Insurance
You may want to see also
Frequently asked questions
What is a deductible?
What is a premium?
What is a policy?
What is a rider?
What is a peril?