The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a federal law that protects the privacy of health and medical information. HIPAA applies to covered entities such as healthcare providers, health plans, healthcare clearinghouses, and business associates. While insurance companies are not covered by HIPAA, they must comply with the law when requesting and accessing an individual's medical records.
When an individual is involved in an accident or injury, the insurance company will often request access to their medical records to evaluate their claim. However, it's important to note that insurance companies are not entitled to an individual's entire medical history and can only access relevant medical records with the individual's authorization. Signing a HIPAA authorization form allows medical providers to release medical information to the insurance company.
Insurance adjusters play a crucial role in this process by reviewing medical records and determining the appropriate amount for the case. However, it is important for individuals to understand their rights under HIPAA and seek legal advice before signing any authorization forms. By understanding HIPAA and its implications, individuals can protect their privacy and control the disclosure of their personal health information.
| Characteristics | Values |
|---|---|
| Does HIPAA apply to insurance adjusters? | Yes, HIPAA applies to insurance adjusters. |
| What is HIPAA? | HIPAA stands for the Health Insurance Portability and Accountability Act of 1996. |
| What does HIPAA do? | HIPAA protects the privacy of an individual's health and medical information. |
| How does HIPAA apply to insurance adjusters? | Insurance adjusters cannot access an individual's medical records without their consent. To grant authorization, individuals must sign a HIPAA authorization form. |
| What information does HIPAA protect? | HIPAA protects "individually identifiable health information", known as protected health information (PHI). This includes details about a person's physical or mental wellness, health services provided to them, and payment for those services. It also includes basic information such as a person's name, address, birthday, and Social Security number. |
| What are the consequences of non-compliance with HIPAA? | Failure to comply with HIPAA can result in monetary penalties or criminal prosecution. |
What You'll Learn
- HIPAA applies to health insurance companies and health information
- Insurance adjusters often request medical records for injury claims
- To access medical records, insurance adjusters need a HIPAA release form
- HIPAA release forms are often broad, allowing access to unrelated records
- Insurance adjusters are not covered by HIPAA and may share medical information

HIPAA applies to health insurance companies and health information

The Health Insurance Portability and Accountability Act (HIPAA) is a federal law that provides baseline privacy and security standards for medical information. The US Department of Health and Human Services (HHS) is responsible for creating rules that implement HIPAA and enforcing them.
HIPAA applies to everyone as individuals, as everyone has personally identifiable health information that they have the right to inspect and request corrections for when errors or omissions exist. However, HIPAA's scope is often misunderstood because the requirement to protect individually identifiable health information is covered in only a small section of a substantial Act.
HIPAA applies to the majority of workers, most health insurance providers, and employers who sponsor or co-sponsor employee health insurance plans. It covers health plans, health care clearinghouses, and health care providers that conduct certain health care transactions electronically to safeguard protected health information (PHI) entrusted to them.
Health plans include health, dental, vision, and prescription drug insurers; health maintenance organizations (HMOs); Medicare, Medicaid, Medicare+Choice, and Medicare supplement insurers; long-term care insurers (excluding nursing home fixed-indemnity policies); employer-sponsored group health plans; government- and church-sponsored health plans; and multi-employer health plans.
Health care providers covered by HIPAA include doctors, clinics, hospitals, psychologists, chiropractors, nursing homes, pharmacies, and dentists—essentially, any entity that provides health care in exchange for payment. These providers must comply with HIPAA if they transmit health information electronically in connection with covered transactions, such as benefit eligibility inquiries, referral authorization requests, and other transactions for which HHS has established standards under the HIPAA Transactions Rule.
Health care clearinghouses are entities that process non-standard health information they receive from another entity into a standard format or vice versa. They rarely deal directly with patients and often act as intermediaries between health care providers and health plans.
In addition to these "covered entities," business associates of covered entities must also follow parts of the HIPAA regulations. Business associates include companies that help administer health plans, process claims, or provide administrative services, billing, payment, and collection services. They also include outside lawyers, accountants, IT specialists, and companies that store or destroy medical records. Covered entities must have contracts in place with their business associates to ensure that they use, disclose, and safeguard health information properly.
The Integrity Tightrope: Examining the Honesty of Insurance Adjusters
You may want to see also

Insurance adjusters often request medical records for injury claims

Insurance adjusters will often request medical records to verify the injuries of the person making the claim. They may also be looking for evidence of previous injuries or conditions that could be used to reduce the amount of compensation they need to pay out. For example, if a claimant has previously suffered a back injury and is now claiming for a back injury as a result of a car accident, the insurance company may try to argue that the current back pain is related to the previous injury.
HIPAA (the Health Insurance Portability and Accountability Act) is a federal law that protects the privacy of individuals' health and medical information. Doctors and medical facilities are required by HIPAA to keep this information private and not disclose it to anyone outside the medical field without the individual's permission.
In the context of insurance claims, this means that insurance adjusters cannot access an individual's medical records without their permission. To grant permission, individuals must sign a HIPAA authorization form. This form allows medical providers to release medical information to the individuals specified on the form.
Protecting your privacy
While insurance adjusters may request access to a claimant's full medical history, they are usually only entitled to view records directly related to the injuries sustained in the accident in question. It is recommended that individuals consult with an attorney before signing a HIPAA authorization form to ensure that they only provide information that is in their best interest. Attorneys can also help individuals to modify authorization forms to limit the medical information they are releasing.
Individuals can also obtain their own medical records and provide them to the insurance company, rather than signing a broad authorization. This allows individuals to know exactly what information is being provided and ensures that irrelevant records are not shared.
In some cases, insurance adjusters may request that claimants undergo an "independent medical examination" (IME) by a physician chosen by the insurance company. However, these examinations are not truly independent, as the doctors are hired and paid by the insurance company and often return opinions that are favorable for the company. Unless required by an injury-related claim under the individual's own insurance policy or a filed personal injury lawsuit, it is recommended that claimants politely refuse to submit to an IME.
Incorporating Lead Safe Practices: A Necessary Evolution in Insurance Adjusting
You may want to see also

To access medical records, insurance adjusters need a HIPAA release form
The Health Insurance Portability and Accountability Act (HIPAA) of 1996 protects the privacy of patients while allowing health data to flow freely between authorized individuals for healthcare activities. HIPAA-covered entities include healthcare providers, health plans, healthcare clearinghouses, and business associates of covered entities.
HIPAA requires a signed release form from a patient before their protected health information can be shared with other individuals or organizations, except in the case of routine disclosures for treatment, payment, or healthcare operations permitted by the HIPAA Privacy Rule.
A HIPAA release form must contain:
- A description of the information to be used/disclosed
- The purpose for which the information will be disclosed
- The name of the person or entity to whom the information will be disclosed
- An expiration date or event when consent is withdrawn
- A signature and date from the individual or their representative, with the relationship to the patient and a description of the representative's authority to act on their behalf
The form must also include statements advising the individual of:
- Their right to revoke authorization
- Any exceptions to this right
- Details of how the authorization can be revoked
- That the covered entity may not condition treatment, payment, enrollment, or eligibility for benefits on whether the individual signs the authorization
- That there is a potential for information disclosed under the terms of the authorization to be redisclosed by the recipient and no longer protected by HIPAA
HIPAA uses a standard of "minimum necessary," meaning that only the information needed to achieve the purpose for which it is being disclosed should be provided.
In the context of insurance adjusters, while an injury victim has the right to refuse to sign a medical release form, doing so will almost certainly result in a denial of their insurance claim. Adjusters often ask claimants to sign a medical release form as they are often not satisfied with copies of accident-related medical records provided by claimants. The scope of the medical release requested by insurance companies is often broader than what is required, as access to a claimant's full medical history gives them more opportunities to deny a claim. However, there is no need for any injury victim to sign a blanket release, and the scope of a signed release should be limited to the treatment of only those injuries sustained during the accident in question.
Understanding Tax Implications: Public Adjuster Payments and Insurance Proceeds
You may want to see also

HIPAA release forms are often broad, allowing access to unrelated records
The Health Insurance Portability and Accountability Act (HIPAA) is a federal law that protects the privacy of health information. It ensures that patients' health information is protected from unauthorized access but can be shared to promote high-quality healthcare.
HIPAA release forms are required when a patient's protected health information is disclosed for any purpose other than treatment, payment, or healthcare operations. These forms are signed by the patient and allow their protected health information to be used by authorized individuals for specific purposes.
HIPAA release forms often include broad language that allows access to all of a patient's medical records, rather than limiting access to specific information relevant to a particular purpose. This can result in insurance companies accessing unrelated medical records and using them to deny or devalue injury claims. For example, they may argue that a previous medical issue contributed to the patient's current injuries.
To avoid this issue, patients can modify the HIPAA release form to limit the medical information they are releasing solely to information related to their current claim. They can also gather their own medical records and provide only the relevant information to the insurance company. Consulting with an attorney before signing a HIPAA release form is generally recommended.
The Ever-Ready Nature of Insurance Adjusters: On-Call Responsibilities
You may want to see also

Insurance adjusters are not covered by HIPAA and may share medical information
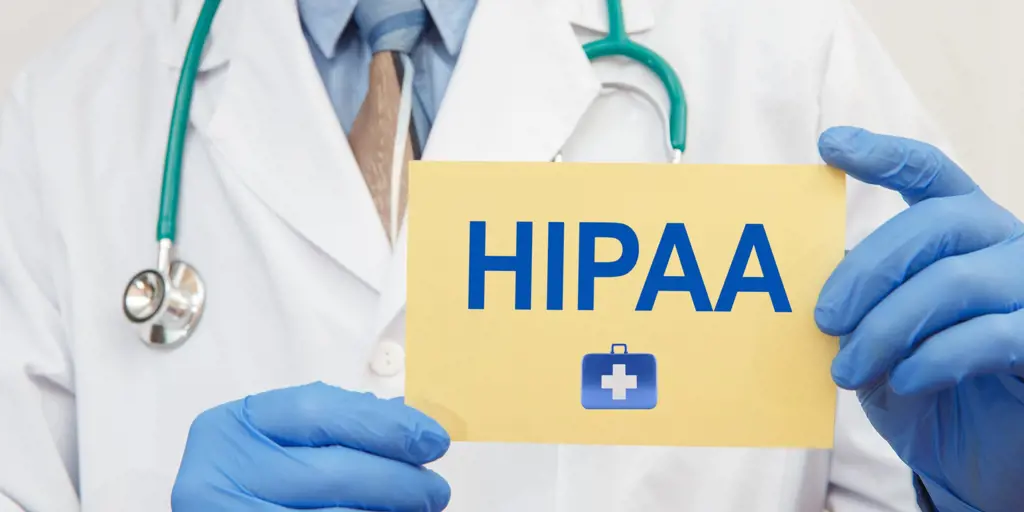
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a federal law that protects the privacy of health and medical information. HIPAA requires national standards to protect sensitive patient health information from being disclosed without the patient's consent or knowledge.
HIPAA applies to "covered entities" such as healthcare providers, health plans, healthcare clearinghouses, and business associates. These are organizations that handle protected health information (PHI) and are required to follow HIPAA regulations.
However, car insurance companies are not considered covered entities under HIPAA. This means that insurance adjusters are not covered by HIPAA and are not legally obligated to maintain the privacy of medical and health information they collect.
When an individual is involved in a car accident, the insurance company of the at-fault driver will often request access to the individual's medical records. The insurance company will ask the individual to sign a Release and Authorization for Disclosure of Health Information under HIPAA. It is important to note that signing this authorization gives the insurance company unlimited access to the individual's medical history, regardless of its relevance to the auto injury.
Since the insurance company is not bound by HIPAA, they can share the individual's medical information with others without their consent. This loss of privacy can be concerning, as it may expose sensitive health information to unauthorized individuals.
To maintain privacy and control over medical and health information, individuals can modify the authorization form provided by the insurance company. They can limit the release of information to only what is relevant to the auto injury and specify the medical providers authorized to release information. Alternatively, individuals can refuse to sign the authorization form and provide the insurance company with only the documentation necessary for their claim evaluation.
In summary, insurance adjusters are not covered by HIPAA and may share medical information if given authorization. However, individuals have the right to control the release of their medical information and can take steps to protect their privacy by modifying or refusing to sign the authorization form.
Insurance Adjusters' Access to Paradise, CA: A Fine Line Between Support and Intrusion
You may want to see also
Frequently asked questions
HIPAA stands for the Health Insurance Portability and Accountability Act of 1996. It is a federal law that establishes national standards and procedures for protecting patients' medical information.
Insurance agents and adjusters are considered “business associates” or "business associate subcontractors" under HIPAA and are therefore required to comply with the law's Privacy and Security Rules.
The Privacy Rule applies to all forms of protected health information (PHI), including electronic, written, and oral formats. It outlines who can use, disclose, or access PHI, which includes basic information such as a person's name, address, birthday, and Social Security number. The Security Rule specifically dictates how to manage electronic PHI (e-PHI) to safeguard it against inappropriate alteration, destruction, or unauthorized access.
Failure to comply with the Privacy Rule can result in monetary penalties or criminal prosecution for both disclosing and obtaining PHI without authorization. Data breaches are a common issue, and sending PHI via unsecured email or leaving voicemails with PHI can potentially qualify as a breach requiring a report and potentially leading to an audit.