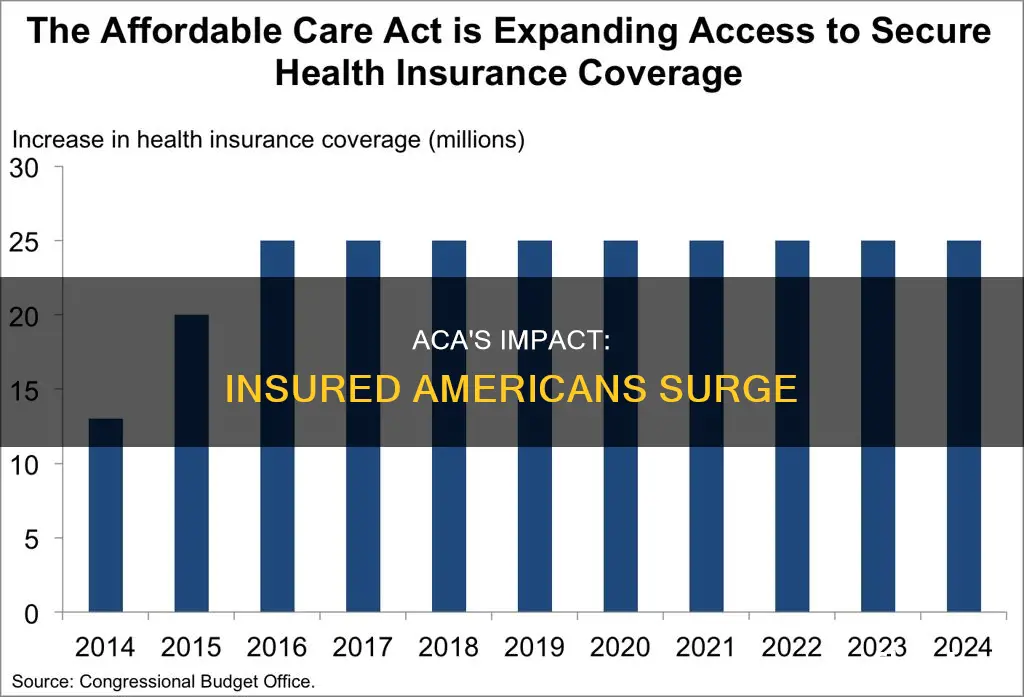
The Affordable Care Act (ACA) has led to a significant increase in the number of people with health insurance coverage in the United States. As of early 2023, over 40 million Americans have health insurance under the ACA, the highest total on record. This includes approximately 18.2 million people with individual market coverage, which is the highest since 2016. The success of the ACA can also be seen in the reduction of uninsured rates across all states, with the national uninsured rate reaching an all-time low of 8.8% in the fourth quarter of 2021. The ACA's expansion of Medicaid to low-income adults and enhanced outreach, streamlined applications, and increased federal funding have been key factors in these gains.
| Characteristics | Values |
|---|---|
| Total number of people enrolled in coverage related to the Affordable Care Act (ACA) | 35 million |
| Uninsured rate in the fourth quarter of 2021 | 8.8% |
| Total number of people enrolled in coverage under the ACA as of early 2023 | 40 million |
| Number of people enrolled in individual market coverage as of early 2023 | 18.2 million |
| Number of people enrolled in ACA Marketplace plans as of February 2021 | 11.3 million |
| Number of people enrolled in Medicaid through the ACA as of December 2020 | 14.8 million |
| Number of people enrolled in the ACA's Basic Health Program | 1 million |
| Number of previously-eligible adult Medicaid enrollees who gained coverage under the ACA | 4 million |
| Number of nonelderly uninsured adults in 2010 | 48.2 million |
| Number of nonelderly uninsured adults in 2016 | 28.2 million |
| Number of people newly insured as a result of the ACA | 20 million |
What You'll Learn
- In 2018, the uninsured rate among US adults aged 19-64 was 12.4%
- The number of underinsured US adults has increased since 2010
- The ACA has expanded coverage options for those without job-based health plans
- The ACA has improved health care access, with more people receiving preventive care and cancer screenings
- The ACA has helped reduce coverage gaps, especially for women and postpartum individuals

In 2018, the uninsured rate among US adults aged 19-64 was 12.4%
In 2018, eight years after the Affordable Care Act (ACA) was passed, the uninsured rate among US adults aged 19-64 was 12.4%. This rate was statistically unchanged from 2016, despite attempts by the Trump administration and Congress to weaken the ACA. While more people have gained insurance under the ACA since 2010, a higher proportion of US adults are now "underinsured", with the sharpest rise in underinsurance occurring among Americans with employer-based health plans.
The 2018 Commonwealth Fund Biennial Health Insurance Survey, which included a nationally representative sample of 4,225 US adults aged 19-64, found that 45% of this age group were inadequately insured. This figure has remained relatively stable since 2010, although there have been important shifts. Firstly, fewer adults are uninsured today compared to 2010, and the duration of coverage gaps has significantly shortened. Secondly, more people who have coverage are now underinsured, with the greatest increase occurring among those in employer plans.
The term "underinsured" refers to insured adults whose out-of-pocket costs over one year (excluding insurance premiums) are equal to 10% or more of their household income. It also includes those whose out-of-pocket costs exceed 5% or more of their household income if they are living under 200% of the federal poverty level, or if their deductible constitutes 5% or more of household income.
People who are underinsured or spend any time uninsured are more likely to experience cost-related problems when trying to access healthcare and have greater difficulty paying medical bills. Having continuous coverage is a significant factor in determining whether people have a regular source of care, receive timely preventive care, or get recommended cancer screenings.
Updating Your Address: A Guide to NAIC Insurance Address Changes
You may want to see also

The number of underinsured US adults has increased since 2010
The Affordable Care Act (ACA) has been instrumental in providing health insurance coverage to millions of Americans. As of early 2022, over 35 million people were enrolled in coverage related to the ACA, with a record-breaking 21 million enrolled in Medicaid expansion coverage. The success of the ACA is evident in the declining uninsured rate, which reached an all-time low of 8.8% in the fourth quarter of 2021.
However, it is important to note that the number of underinsured US adults has increased since 2010. While more people have gained health insurance under the ACA, a higher proportion of adults are now considered underinsured. This means that they have health insurance but still face challenges in accessing affordable and comprehensive healthcare.
The Commonwealth Fund's Biennial Health Insurance Survey in 2018 revealed that 45% of US adults aged 19 to 64 were inadequately insured. This proportion has remained relatively unchanged since 2010, but the number of underinsured individuals has grown. The greatest increase in the underinsured rate was observed among Americans with employer-based health plans.
The rise in underinsurance is attributed to various factors. Firstly, the ACA primarily focused on expanding coverage for those without insurance, while employer-based plans remained largely unchanged. As a result, the cost-sharing requirements and high deductibles associated with employer-sponsored insurance have contributed to the increase in underinsured individuals.
Additionally, the rising cost of healthcare has outpaced income growth, making it challenging for individuals to afford out-of-pocket expenses and high deductibles. This is particularly true for those with moderate incomes, who may not qualify for subsidies or cost-sharing reductions. Furthermore, the complexity and cost of regulations have led to a loss of employer-sponsored insurance for millions of people.
The consequences of being underinsured can be significant. Underinsured individuals often face unaffordable medical bills and are more likely to delay or forgo necessary healthcare due to financial constraints. They may struggle with medical debt and experience negative financial consequences, such as using up savings or borrowing money.
Addressing the issue of underinsurance is crucial for ensuring that individuals have access to affordable and comprehensive healthcare. Policy interventions, such as expanding Medicaid, improving cost-sharing reductions, and enhancing protections for those with employer-sponsored insurance, can help mitigate the challenges faced by the underinsured.
Informed Policy Changes: Notify Pendon
You may want to see also

The ACA has expanded coverage options for those without job-based health plans
The Affordable Care Act (ACA) has expanded coverage options for those without job-based health plans. If you are unemployed, you may be able to get an affordable health insurance plan through the Marketplace, with savings based on your income and household size. Your household size and income determine your eligibility for health coverage and the amount of financial help you will get when paying for coverage.
If you have lost your job and your job-based insurance, you qualify for a Special Enrollment Period. This means you can enroll in a Marketplace insurance plan at any time of year, usually within 60 days of losing your coverage.
There is no limited enrollment period for Medicaid or the Children's Health Insurance Program (CHIP). If you qualify, you can enroll in these programs at any time of year. You can also qualify for free or low-cost coverage through these programs.
If you are eligible for coverage under a family member's job-based plan but choose to get a Marketplace plan instead, you may not be able to get lower costs on your Marketplace coverage based on your income. This depends on whether the job-based insurance that is offered to you is considered affordable and meets certain minimum standards.
If you get a new job that does not offer insurance, you can keep your Marketplace plan and may qualify for lower costs based on your household size and income.
Juggling Dual Coverage: Navigating Billing for Two Insurances
You may want to see also

The ACA has improved health care access, with more people receiving preventive care and cancer screenings
The Affordable Care Act (ACA) has improved access to healthcare in the US, with more people receiving preventive care and cancer screenings.
Before the ACA, the age group most likely to be uninsured were 18-24 year olds. In 2009, nearly 9.7 million people in this age group didn't have health insurance. After the ACA was introduced, the number of uninsured people in this age group dropped to 4.7 million by 2018. This meant that more 19-25-year-old people diagnosed with cancer had health insurance than before the ACA.
The ACA has also helped improve the quality of cancer care for young adults. One study found a significant decrease in late-stage cervical cancer diagnoses for women aged 21-25 after the ACA took effect, compared to 26-34-year-old women who were not eligible to remain on their parents' health insurance. There was also an increase in the number of women aged 19-25 who got vaccinated for HPV, which is the most important risk factor for developing cervical cancer.
In addition to helping young people, the ACA has also helped to reduce disparities in health insurance coverage for cancer care, particularly for racial and ethnic minorities, people with low incomes, and people who live in rural areas. Through the ACA, the number of uninsured cancer patients in expansion states declined more for these groups.
The ACA has also made many preventive health services free, including cancer screenings such as colonoscopies and mammograms. This has helped people who are trying to prevent cancer or detect it early. One study found that the rate of women getting a mammogram increased by up to 9% when cost-sharing was removed.
Overall, the ACA has transformed the US healthcare system, providing coverage for millions of Americans and protecting people with pre-existing conditions.
Adjusting Root Insurance Payment Day: A Guide
You may want to see also

The ACA has helped reduce coverage gaps, especially for women and postpartum individuals
The Affordable Care Act (ACA) has been instrumental in reducing coverage gaps, especially for women and postpartum individuals. The ACA's coverage expansions in 2014 marked the most significant expansion in US history since the establishment of Medicare and Medicaid in 1965.
One of the most notable impacts of the ACA has been the reduction in uninsurance rates among reproductive-aged women. From 1980 to 2009, the rate of uninsurance among this group steadily increased, with one in four women of reproductive age lacking insurance by 2009. The ACA's coverage expansions helped reverse this trend, leading to a significant reduction in uninsurance rates. By 2018, the uninsured rate among US adults aged 19 to 64 was 12.4%, remaining unchanged from 2016 despite attempts by the Trump administration and Congress to weaken the law.
The ACA has also improved access to care for women, particularly those with lower incomes. Among reproductive-aged women, the ACA was associated with a decrease in the probability of uninsurance and an increase in Medicaid and nongroup private coverage. It also led to a reduction in cost-related barriers to medical care and an increase in having a usual source of care.
The ACA's impact on pregnant women is more nuanced. While there were no significant changes in insurance status or access to care for this group in the immediate years following the ACA's implementation, the law did improve timing and uptake of Medicaid coverage for pregnant women eligible for pregnancy-related Medicaid. Additionally, the ACA's coverage provisions expanded coverage options for women losing pregnancy-related Medicaid/CHIP coverage postpartum.
The ACA's major coverage provisions, such as Medicaid expansion and subsidized plans available through the Marketplaces, have contributed to gains in coverage and affordability of services for pregnancy-related care, both pre- and postpartum. The law established a floor for "essential health benefits" that individual market plans must cover, including maternity care, which was often excluded before the ACA. The ACA also mandates that all private plans and Medicaid expansion programs cover routine pregnancy screenings and vitamins at no cost.
Furthermore, the ACA addresses affordability challenges faced by women, who on average use the health system more and have higher health expenses than men. The law requires plans to cap annual out-of-pocket charges and has eliminated cost-sharing for preventive services, including prenatal tests, breastfeeding services, mammograms, and contraception. As a result, out-of-pocket spending for contraceptives has plummeted since the ACA went into effect.
In summary, the ACA has played a crucial role in reducing coverage gaps for women and postpartum individuals. It has expanded access to insurance, improved affordability of services, and enhanced continuity of care, leading to better health outcomes for these vulnerable populations.
Understanding PL Promise Term 10 Insurance: A Comprehensive Guide
You may want to see also
Frequently asked questions
Over 30 million people have gained health coverage through the Affordable Care Act (ACA).
CAC refers to the Affordable Care Act, also known as Obamacare.
As of 2021, the uninsured rate in the US was 8.8%.
The number of people with health insurance has increased since the ACA was implemented in 2014. For example, in 2018, eight years after the ACA was passed, the uninsured rate among US adults aged 19 to 64 was 12.4%, compared to 15.5% in 2010.
The ACA's expansion of Medicaid to low-income adults under 65 has resulted in over 20 million people gaining Medicaid coverage.