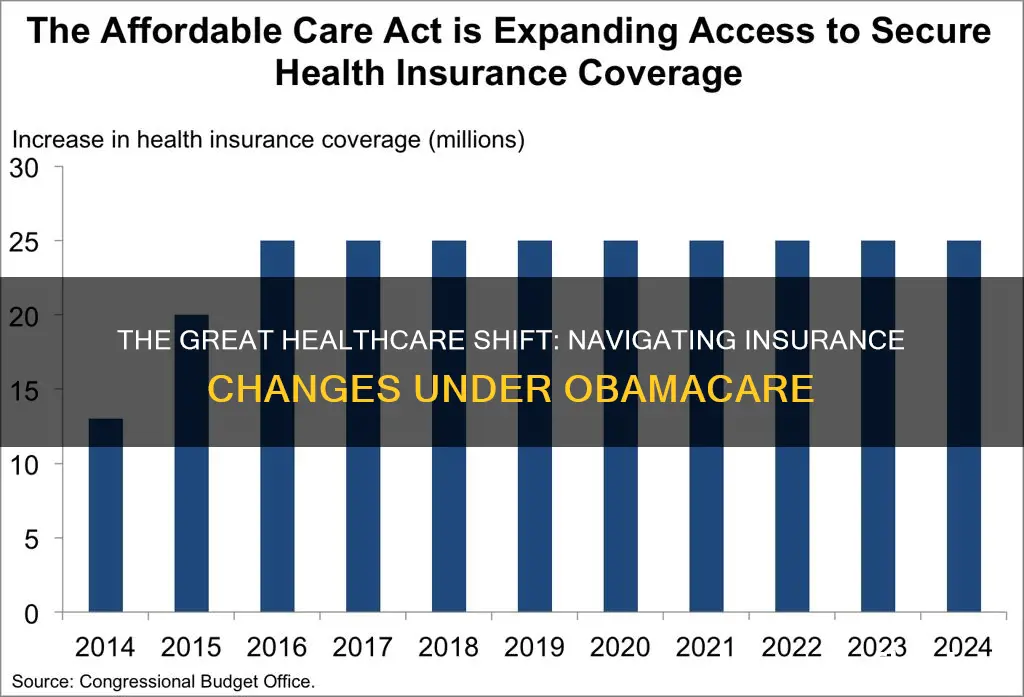
The Affordable Care Act (ACA), commonly referred to as Obamacare, has led to millions of people gaining health coverage. In 2022, over 35 million people enrolled in coverage related to the ACA, with 21 million of those enrolled in Medicaid expansion coverage. This has resulted in the uninsured rate in the US reaching an all-time low of 8.8% in the fourth quarter of 2021. However, it is important to note that the number of people who remained without coverage increased by half a million in 2017, and there have been concerns about the impact of Obamacare on existing insurance plans.
What You'll Learn

The number of people who had to change their insurance plans under Obamacare
The Affordable Care Act (ACA), commonly referred to as Obamacare, was signed into law by President Barack Obama in 2010. It extended health insurance coverage to millions of Americans, and the uninsured rate dropped to a historic low in 2016. However, the number of people remaining without coverage increased by half a million in 2017, reaching 27.4 million.
The ACA's impact on insurance plans was a significant point of contention. One of the key promises made by President Obama and his administration was that citizens could keep their existing health insurance plans if they liked them. However, the reality was more complex. While plans created before the enactment of the ACA were allowed to remain in effect until they underwent significant changes, plans created between 2010 and 2014 had to comply with the law's requirements by the beginning of 2014. This included a requirement that insurance plans cover a standard set of essential benefits.
As a result, many people who had purchased individual health insurance plans received notifications that their current plans would be canceled and replaced with new plans that met the ACA's minimum coverage requirements. It is estimated that between 50% and 75% of the 14 million Americans with individual health insurance plans were likely to receive cancellation notices over 2014. This led to a backlash, with the Obama administration offering a fix in November 2013 to allow people to keep their existing plans for another year.
The impact of the ACA on insurance plans extended beyond the individual market. Analysis by the American Enterprise Institute predicted that between 50% and 66% of small businesses would have their employee insurance policies canceled or choose to drop coverage due to the benefits mandate, potentially affecting up to 100 million small and large business plans.
In conclusion, while the exact number of people who had to change their insurance plans under Obamacare is challenging to pinpoint, it is clear that a significant number of Americans experienced changes to their existing plans due to the implementation of the ACA.
Unraveling the Mystery of Calculating HLV for Term Insurance: A Comprehensive Guide
You may want to see also

The impact of Obamacare on insurance premiums
The Affordable Care Act (ACA), or Obamacare, was signed into law by President Barack Obama in 2010. The ACA's primary goal was to slow the rising cost of healthcare by making health insurance more available and affordable.
The Early Effects of the ACA on Premiums
The ACA created online exchanges where consumers could shop for comparable health insurance plans. The law also established a mandate to purchase health insurance, bringing more healthy young people into the market and putting downward pressure on healthcare costs.
The ACA included several provisions aimed at improving the quality of individual plans. For example, insurers were required to cover policyholders with pre-existing medical conditions and to provide certain "essential benefits", such as maternity and mental health coverage. While these components of the ACA could have pushed premiums higher, the policies Americans are buying today offer greater benefits—including a cap on out-of-pocket expenses—than those purchased before the ACA.
In the second year of the online exchanges (2015), the Kaiser Family Foundation found that price increases were fairly small. Nationwide, premiums for exchange-based plans with a medium level of coverage rose by a modest 2%—without accounting for the effect of subsidies that reduce out-of-pocket expenses for some individuals and families.
More Recent Effects of the ACA on Premiums
In 2018 and 2019, the ACA's marketplaces experienced turmoil, resulting in huge premium swings. In 2018, the lowest silver marketplace premium offered in each rating region increased sharply by 29.7% on average. Twenty-eight states increased their average lowest silver premium by more than 29%.
However, in 2019, many insurers realized they had overreacted, and increases for the lowest silver premiums averaged -0.4% nationwide, and, in many states, premiums decreased. In 2020, continued stability caused premiums to fall across all states by an average of 3.5%.
The Impact of the ACA on Insurance Premiums in 2022
The ACA made premium tax credits available to people purchasing health coverage on the marketplaces but only when their incomes fell between 100% and 400% of the federal poverty level. As a result, millions of uninsured people became eligible for subsidized coverage.
The Inflation Reduction Act of 2022 enabled those with incomes of 100% to 150% of the poverty level to be eligible for free or nearly free silver plans. But even with the subsidies provided by the act, Silver plans increased by 4.1%. Bronze plans increased in price by 4.0%, and Gold plans by 2.2%.
Overall Impact of the ACA on Insurance Premiums
While the results vary from state to state, the overall numbers suggest that post-ACA premium increases have fluctuated but have been modest compared to those before ACA implementation.
The ACA has accomplished what it was designed to do, making healthcare available for more people. However, it is important to note that a higher share of U.S. adults are now "underinsured", with the greatest growth in the underinsured rate occurring among Americans in employer-based health plans.
Understanding LACP: Unraveling the Mystery of Insurance Acronyms
You may want to see also

The effect of Obamacare on the uninsured rate
The Affordable Care Act (ACA), commonly known as Obamacare, has had a significant impact on the uninsured rate in the United States. Before the ACA, the number of uninsured Americans increased over time, especially during economic downturns. By 2013, the year before the ACA's major coverage provisions took effect, more than 44 million people were uninsured.
Under the ACA, millions of people gained health coverage, and the uninsured rate dropped to a historic low. The most significant decline in the uninsured rate occurred among low-income individuals, people of colour, and adults—groups that historically had high uninsured rates. Additionally, the ACA's expansion of Medicaid to low-income adults under 65 played a crucial role in reducing the uninsured rate.
However, there was a slight increase in the number of uninsured people in 2017, reaching 27.4 million. This was the first time the number rose since the implementation of the ACA. Despite this setback, the overall trend showed a decrease in the uninsured rate.
During the coronavirus pandemic, the coverage expansions put in place by the ACA served as a vital safety net for those who lost their jobs or faced economic hardships. The continuous enrollment provision in Medicaid and enhanced subsidies in the Marketplace further protected low-income individuals and improved the affordability of private coverage. As a result, the uninsured rate continued its downward trend, reaching a record low of 9.6% in 2022.
The success of the ACA in reducing the uninsured rate is evident in the latest data. In early 2023, the national uninsured rate reached an all-time low of 7.7%. Approximately 6.3 million people gained health coverage since 2020, coinciding with the start of the Biden-Harris Administration. The enhanced Marketplace subsidies, continuous enrollment in Medicaid, and recent state Medicaid expansions contributed significantly to this achievement.
While there have been fluctuations, the overall trend since the implementation of the ACA has been a steady decrease in the uninsured rate. This reduction in the uninsured rate demonstrates the positive impact of policy interventions on expanding health coverage and improving access to healthcare for millions of Americans.
Understanding Barratry in Insurance: Navigating the Fine Line Between Fraud and Persuasion
You may want to see also

The impact of Obamacare on healthcare access
The Affordable Care Act (ACA), also known as Obamacare, has had a profound impact on healthcare access in the United States. The ACA's primary goal was to expand health insurance coverage and make it more affordable for millions of Americans. Here are some key ways in which the ACA has impacted healthcare access:
- Expanding health insurance coverage: The ACA expanded eligibility for Medicaid, allowing more individuals to access healthcare services. It also established Health Insurance Marketplaces, making it easier for individuals and small businesses to shop for and compare insurance plans.
- Protecting consumers: The ACA introduced provisions to protect consumers, such as prohibiting insurance companies from denying coverage based on pre-existing conditions and mandating essential health benefits.
- Controlling healthcare costs: The ACA implemented measures to control healthcare costs, including promoting competition through Health Insurance Marketplaces and requiring insurance plans to cover essential health benefits.
- Improving access to healthcare: The ACA enhanced access to healthcare by expanding Medicaid and allowing young adults to remain on their parents' insurance plans until age 26. It also ensured coverage for pre-existing conditions and provided essential health benefits.
- Enhancing affordability: The ACA provided premium subsidies and cost-sharing reductions, making insurance coverage more affordable for individuals and families. It also expanded Medicaid eligibility and included provisions to reduce prescription drug costs.
- Improving quality of care: The ACA introduced initiatives like Accountable Care Organizations and value-based payment models to improve care coordination and quality outcomes. It also mandated coverage for preventive services and established programs for quality reporting and transparency.
Despite these positive impacts, the ACA has faced challenges, including political and legal debates, rising healthcare costs, and health disparities. Ensuring universal access and affordability remains a complex task. The future of the ACA depends on ongoing evaluation, innovation, and collaboration to address these challenges and improve healthcare access, affordability, and quality for all.
LIC vs. Term Insurance: Unraveling the Best Option for Your Peace of Mind
You may want to see also

The effect of Obamacare on healthcare quality
The Affordable Care Act (ACA), or Obamacare, was the most significant change in US health care policy since the passage of Medicaid and Medicare in 1965. The ACA's three primary goals were to increase the number of insured, improve the quality of care, and reduce the costs of health care.
The ACA has been successful in increasing the number of insured. The law generated one of the largest expansions of health coverage in US history, with about 20 million more Americans gaining health insurance coverage since the ACA was enacted. The number of uninsured people in the US dropped to a historic low of 9% in 2016, though this number has since increased.
The ACA has also improved access to care for those who gained coverage. People who gained health coverage are more likely to report having a usual place of care. The ACA has also improved access to prescription drugs, particularly for low-income Americans.
The ACA has had a mixed impact on the quality of health care services. While the law has improved access to care, it has not improved the quality of that care. The ACA has not led to a reduction in overall health care costs, and out-of-pocket costs remain a barrier to accessing care for many.
The ACA has also had a positive impact on health outcomes for some groups. For example, Medicaid expansion has been associated with reductions in deaths from cardiovascular-related causes and end-stage renal disease among middle-aged adults. The ACA has also improved health outcomes for people with chronic conditions such as diabetes.
Overall, the ACA has had a positive impact on healthcare quality by increasing the number of insured and improving access to care and prescription drugs. However, the law has had a more limited impact on reducing healthcare costs and improving the quality of care.
Frequently asked questions
It is hard to say exactly how many people had to change their insurance under Obamacare, but millions of people gained health coverage, and the uninsured rate dropped to a historic low.
By 2013, the year before the major coverage provisions of Obamacare went into effect, more than 44 million people lacked coverage.
The uninsured rate dropped to a historic low of 8.8% in 2021, with more than 35 million people enrolled in coverage related to Obamacare.