Pancreatitis is a painful inflammation of the pancreas, which can have serious health consequences, including death. The pancreas is a large gland located behind the stomach and intestines, which produces digestive enzymes and hormones, including insulin, to regulate blood sugar. Pancreatitis can be acute, a sudden onset of inflammation, or chronic, a long-term degeneration. The condition is difficult to diagnose and treat due to the pancreas's location in the abdomen, but it is usually caused by gallstones or alcohol use. The complications of pancreatitis, especially chronic pancreatitis, can be life-threatening, and may result in diabetes, malnutrition, and pancreatic cancer. This makes it a high-risk condition for life insurance companies, and sufferers may struggle to find affordable coverage.
| Characteristics | Values |
|---|---|
| Type of pancreatitis | Acute or chronic |
| Cause | Gallstones, alcohol use, abdominal injury, certain medications, family history, high calcium levels in the blood, high triglyceride levels in the blood, infections, autoimmune disease, inherited gene mutations, complications of cystic fibrosis |
| Symptoms | Abdominal pain, nausea, vomiting, fast shallow breathing, indigestion, loss of appetite, unintended weight loss, fatty stools, lightheadedness, abdominal distension or bloating, tachycardia, severe thirst, dehydration |
| Complications | Necrotizing pancreatitis, cysts and infections, pancreatic cancer, diabetes |
| Diagnosis | Blood tests, CT scans, abdominal ultrasounds, endoscopic retrograde cholangiopancreatography (ERCP), magnetic resonance cholangiopancreatography (MRCP) |
| Treatment | IV fluids, tube feeding, parenteral nutrition, pain relief, gallbladder removal surgery, pancreatic enzyme supplements, insulin, vitamin supplements, lifestyle changes |
What You'll Learn
- Pancreatitis is a pre-existing condition, so insurance companies will consider you a high risk
- Acute pancreatitis can be treated with rest, hydration and pain relief
- Chronic pancreatitis is a permanent condition that requires ongoing treatment
- The pancreas cannot heal itself, so it's important to reduce stress on the organ
- The main risk factors for chronic pancreatitis are drinking and smoking

Pancreatitis is a pre-existing condition, so insurance companies will consider you a high risk
Pancreatitis is a serious condition that can have life-threatening complications. It is caused by inflammation of the pancreas, a large gland located behind the stomach and intestines. The pancreas is responsible for producing digestive enzymes and hormones, including insulin, which regulates blood sugar levels. When the pancreas becomes inflamed, it can lead to severe abdominal pain, nausea, vomiting, and even weight loss.
There are two types of pancreatitis: acute and chronic. Acute pancreatitis is a sudden onset of inflammation that may last for a few days and then go away without treatment. However, recurring attacks of acute pancreatitis can cause damage to the pancreas and lead to chronic pancreatitis, which is a long-term degeneration of the organ. Scar tissue formation on the pancreas can cause the gland to function improperly, resulting in digestive problems and diabetes.
The complications associated with pancreatitis, especially chronic pancreatitis, can be severe and even life-threatening. These include cysts and infections that may require surgery. In some cases, pancreatitis can lead to pancreatic insufficiency, where the pancreas loses its ability to produce enough digestive enzymes, resulting in malnutrition. Additionally, chronic inflammation increases the risk of pancreatic cancer.
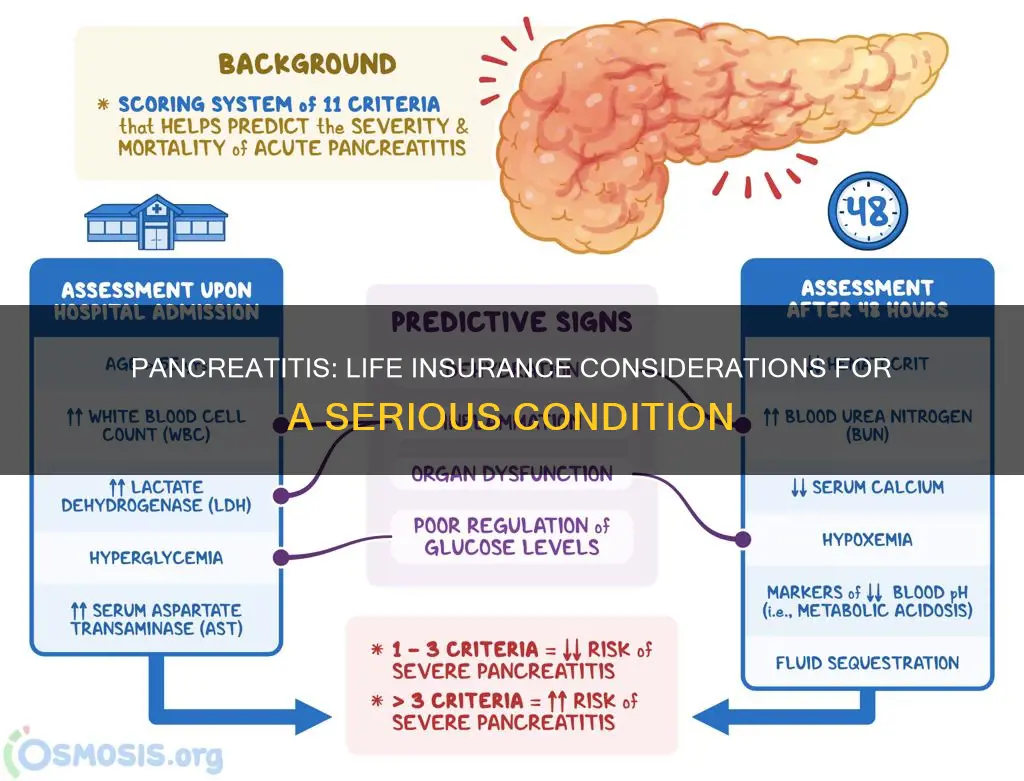
Due to the potential severity of pancreatitis and its impact on the body's major functions, insurance companies consider it a pre-existing condition and view applicants with a history of pancreatitis as high-risk individuals. The condition affects everyone differently, and the assessment process involves a thorough investigation into the applicant's medical history. Insurance underwriters will consider factors such as the frequency and severity of attacks, underlying health conditions, and family history.
While individuals with acute pancreatitis may receive more favorable ratings and affordable premiums, those with chronic pancreatitis will likely be rated as sub-standard and face higher premiums. The assessment will depend on the underlying health condition causing the pancreatitis, with genetic causes generally viewed more favorably than those related to alcohol consumption or other serious health issues.
Life Insurance: Expensive or Affordable?
You may want to see also

Acute pancreatitis can be treated with rest, hydration and pain relief
Acute pancreatitis is a temporary condition that can be treated with rest, hydration, and pain relief. It occurs when the pancreas is attempting to recover from a minor, short-term injury. Most people with acute pancreatitis will recover completely within a few days with supportive care.
Rest
Acute pancreatitis is treated in the hospital, where patients are closely monitored for signs of serious problems and given supportive treatment. Patients with mild acute pancreatitis usually start to get better within a week and experience no further problems or improvements within 48 hours. Many people are well enough to leave the hospital after a few days. However, those with severe acute pancreatitis can develop complications that require further treatment and may need to be admitted to a high-dependency unit or intensive care unit (ICU).
Hydration
Acute pancreatitis often causes dehydration, so fluids are typically given through a tube into the patient's vein (intravenous or "IV" fluid) to prevent this. In the early phase of the illness, aggressive fluid resuscitation is critically important. This can be done through crystalloids or colloids, with the goal of maintaining hemodynamic stability. This usually involves the administration of several litres of fluid as a bolus, followed by continuous infusion at a rate of 250-500 mL/h. Central venous pressure, pulmonary artery wedge pressure, and urine output can be monitored to ensure adequate hydration.
Pain Relief
Acute pancreatitis often causes severe abdominal pain, so patients are usually given painkillers. In addition, if the patient has an infection in addition to pancreatitis, such as a chest or urinary infection, antibiotics may be necessary.
Life Insurance Exam Frequency: How Often is the NC Exam?
You may want to see also

Chronic pancreatitis is a permanent condition that requires ongoing treatment
Lifestyle Changes
It is crucial for individuals with chronic pancreatitis to stop consuming alcohol, even if alcohol is not the cause of their condition. Abstaining from alcohol can prevent further damage to the pancreas and may reduce the pain associated with the condition. Additionally, it is recommended to quit smoking, as smoking can accelerate the damage caused by chronic pancreatitis, increasing the likelihood of the pancreas ceasing to function.
Dietary Changes
As chronic pancreatitis can impact the ability to digest certain foods, dietary changes are often necessary. A low-fat, high-protein, and high-calorie diet is usually recommended, along with fat-soluble vitamin supplements. However, it is important to consult a healthcare professional before making any significant dietary changes.
Medication
Pain relief is an important aspect of treating chronic pancreatitis. Over-the-counter medications such as paracetamol or anti-inflammatories like ibuprofen are typically the first line of treatment. If these medications are ineffective, stronger painkillers, such as opiate-based painkillers, may be prescribed. Additionally, pancreatic enzyme supplements are often recommended to support the digestive system.
Surgery
In more severe cases, surgery may be required to relieve pain or treat complications. Endoscopic surgery, such as lithotripsy, can be used to break down gallstones, and a procedure called a pancreas resection involves surgically removing inflamed parts of the pancreas. In the most severe cases, a total pancreatectomy may be necessary, involving the removal of the entire pancreas.
Failing Life Insurance Blood Tests: What You Need to Know
You may want to see also

The pancreas cannot heal itself, so it's important to reduce stress on the organ
Pancreatitis is an inflammatory disorder of the pancreas that can cause life-threatening complications. The pancreas is an organ in the abdomen that sits between the stomach and the spine. It is involved in digestion and regulating blood sugar by producing digestive enzymes and hormones like insulin.
While acute pancreatitis is temporary and most people recover completely in a few days, chronic pancreatitis is a long-term, progressive condition that gets worse over time. It happens when the injury or damage to the pancreas is constant and never stops. This constant inflammation causes scarring of the pancreas tissues, which stops them from making enzymes and hormones.
The pancreas cannot heal itself, so it is important to reduce stress on the organ. Here are some ways to do that:
- Avoid alcohol and tobacco: Alcohol is a leading cause of both acute and chronic pancreatitis. Avoiding alcohol and quitting smoking can help reduce stress on the pancreas and slow down the progression of the disease.
- Eat smaller meals: Eating smaller meals more frequently can help alleviate physical symptoms associated with exocrine pancreatic insufficiency (EPI), which is a common complication of chronic pancreatitis.
- Maintain a healthy diet: It is important to stick to a healthy diet that is low in fat and protein. Greasy and fried foods can aggravate EPI symptoms.
- Take pancreatic enzyme replacement therapy (PERT): PERT replaces the body's missing pancreatic enzymes. It is important to take PERT as prescribed, with every meal and snack, to help alleviate symptoms.
- Stay hydrated: Drinking plenty of water is crucial. Staying hydrated can help prevent dehydration, which can occur with diarrhea, a common symptom of EPI.
- Manage stress: Chronic stress can increase the susceptibility of the pancreas to inflammatory diseases. Practicing stress-management techniques like meditation or deep breathing can help reduce stress levels and improve quality of life.
- Seek emotional support: EPI can interfere with daily life and cause stress and anxiety. Confiding in loved ones and joining support groups can provide critical emotional support and help with staying on track with dietary changes and medications.
By taking these steps to reduce stress on the pancreas, individuals with pancreatitis can better manage their condition and slow down its progression.
Fegli Life Insurance: When to Expect Payouts?
You may want to see also

The main risk factors for chronic pancreatitis are drinking and smoking
Drinking alcohol is the most common cause of pancreatitis. Alcohol use is linked to around half of both acute and chronic pancreatitis cases. Alcohol can cause acute pancreatitis by sensitising the pancreas to other injuries or insults. This can lead to chronic pancreatitis as the inflammation gets worse over time. The amount and duration of alcohol consumption are the most important factors in increasing the risk of pancreatitis. Drinking heavily is associated with a higher risk of developing pancreatitis, with the risk increasing with the amount of alcohol consumed. However, even smaller amounts of alcohol can increase the risk, and individuals who have had an episode of alcohol-related pancreatitis should avoid alcohol consumption to prevent disease progression.
Smoking is also an independent risk factor for chronic pancreatitis and has a synergistic effect with alcohol. It is a dose-dependent risk factor, meaning that the risk of pancreatitis increases with the amount of smoking. Current smokers have a higher risk of developing pancreatitis compared to former smokers. Smoking cessation can help reduce the risk of pancreatitis and prevent disease progression.
In addition to drinking and smoking, other risk factors for pancreatitis include gallstones, infections, autoimmune diseases, hereditary factors, high blood triglyceride levels, and certain medications.
Canceling Freedom Life Health Insurance: A Step-by-Step Guide
You may want to see also
Frequently asked questions
Pancreatitis is an inflammation of the pancreas, a large gland located in the abdomen. The pancreas has two main functions: producing digestive enzymes and producing hormones that regulate blood sugar. Pancreatitis can be acute (short-term and sudden) or chronic (long-term).
The primary symptom of pancreatitis is abdominal pain, which may radiate to the back. Other symptoms include nausea, vomiting, fast heart rate, severe thirst or dehydration, and unintended weight loss. Chronic pancreatitis can lead to malnutrition, diabetes, and pancreatic cancer.
The most common causes of pancreatitis are gallstones and alcohol use. Other causes include abdominal injury or surgery, certain medications, high calcium or triglyceride levels in the blood, and genetic factors such as cystic fibrosis.
Treatment for pancreatitis depends on the type, severity, and cause. Acute pancreatitis usually involves supportive care such as IV fluids, tube feeding, and pain relief. Chronic pancreatitis treatment includes pancreatic enzyme supplements, insulin, vitamin supplements, and lifestyle changes such as quitting alcohol and smoking.
Pancreatitis is considered a high risk by life insurance companies due to its potential life-threatening complications. Individuals with pancreatitis may be assessed a Sub-Standard rating with high premiums or even be declined if insufficient information is provided. However, those with acute pancreatitis caused by non-serious factors and overall good health may receive the best health class ratings with lower premiums.