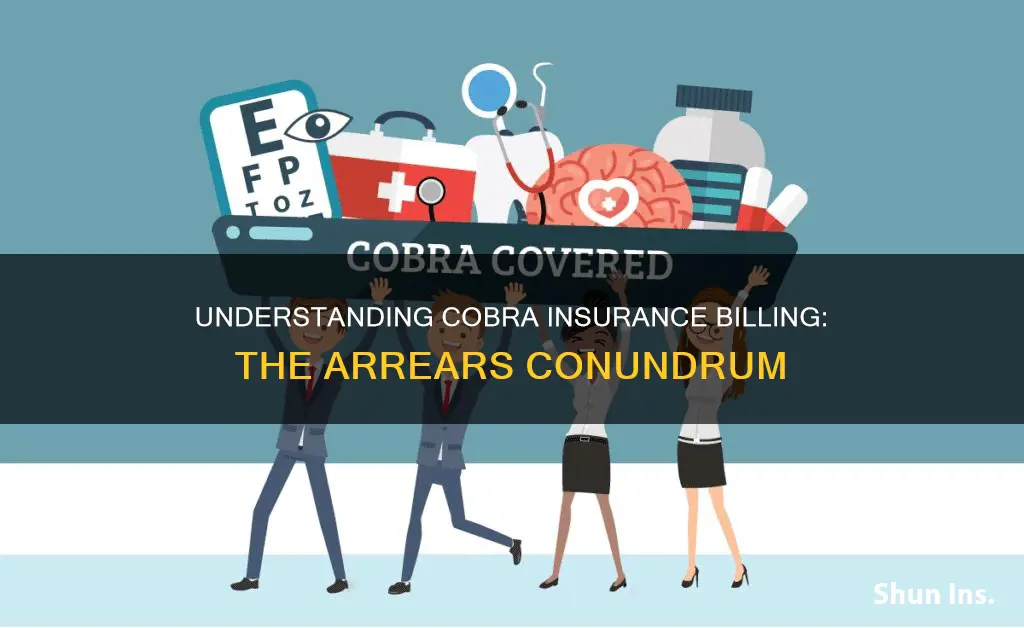
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal law that allows eligible employees and their dependents to retain their health insurance coverage for a limited period after losing their job or experiencing a reduction in work hours. COBRA is available to those enrolled in an employer-sponsored medical, dental, or vision plan, whose former company has 20 or more full-time employees. While COBRA can be expensive, it provides an insurance safety net between jobs and allows individuals to maintain their existing coverage for pre-existing conditions and regular prescription drugs.
| Characteristics | Values |
|---|---|
| What is COBRA? | Consolidated Omnibus Budget Reconciliation Act |
| Who does COBRA apply to? | Employers with 20 or more full-time employees |
| Who is eligible for COBRA? | Former employees, spouses, former spouses, and dependent children |
| How long does COBRA coverage last? | 18 or 36 months |
| What is the cost of COBRA coverage? | The full cost of the insurance premium plus an additional 2% for administrative costs |
| How soon must you decide whether to elect COBRA coverage? | 60 days from a "qualifying event" or the date your notice is mailed |
| What is a "qualifying event"? | Job loss, divorce, death of a spouse, reduction in work hours, etc. |
What You'll Learn
- COBRA insurance is available to eligible employees and their dependents
- COBRA is applicable to employers with 20 or more full-time employees
- Qualifying events for COBRA include termination, reduction in hours, divorce, death, and Medicare eligibility
- COBRA coverage lasts for 18 or 36 months, depending on the scenario
- COBRA is a federal statute, and non-compliance can be reported to the U.S. Department of Labor

COBRA insurance is available to eligible employees and their dependents
To be eligible for COBRA, employees must have been enrolled in a company-sponsored group health insurance plan on the day before the qualifying event, and the insurance plan must have been effective on more than 50% of the employer's typical business days in the previous calendar year. The qualifying event must result in a loss of the employee's health insurance.
Qualifying events for employees include voluntary or involuntary job loss (except in cases of gross misconduct) and a decrease in the number of hours of employment resulting in a loss of employer insurance coverage. Qualifying events for spouses include the covered employee becoming entitled to Medicare, divorce or legal separation from the covered employee, and death of the covered employee. Qualifying events for dependent children are the same as for spouses, with the addition of loss of dependent child status as per the plan rules.
COBRA coverage is available for a limited period of 18 or 36 months, depending on the applicable scenarios. The cost of COBRA coverage is typically higher than the cost of insurance during employment because the individual must pay the full amount of the insurance premium, including the portion previously covered by the employer and their own prior contribution. This can range from $400 to $700 per individual per month.
COBRA is a convenient option for retaining health insurance after losing employer-sponsored benefits, but it is important to weigh the pros and cons and explore alternative options to find the best fit for your needs.
Navigating the Insurance Billing Process: Understanding Patient Copays
You may want to see also

COBRA is applicable to employers with 20 or more full-time employees
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal law that allows employees to continue their health insurance coverage for a limited period after a change in eligibility. This could be due to voluntary or involuntary job loss, a reduction in hours, divorce, death, or other life events.
COBRA is designed to provide an insurance safety net for those who lose their job or experience a reduction in work hours. It allows eligible employees and their dependents to continue their health insurance coverage, including prescription drugs, dental treatments, and vision care.
Under COBRA, employers are required to offer the same group health insurance plan that the employee had while working. This means that the employee can continue to see the same physicians and medical providers, and maintain coverage for pre-existing conditions and regular prescriptions.
The cost of COBRA coverage is typically higher than the cost of insurance during employment because the individual must pay the full amount of the insurance premium, including the portion previously covered by the employer. In addition, employers are allowed to charge an administrative fee of up to 2% on top of the full cost of the premium.
To be eligible for COBRA, an employee must have been enrolled in a company-sponsored group health insurance plan on the day before the qualifying event. The qualifying event must result in a loss of health insurance coverage.
COBRA provides a temporary extension of health coverage, usually for 18 months, but this can be extended to 36 months in certain circumstances.
While COBRA can be expensive, it may be worth paying for to prevent a gap in health insurance coverage. It is important for individuals to weigh the pros and cons of COBRA and compare it to other available individual plans to select the best option for their needs.
**Understanding Insurance Reimbursement: The Insured's Path to Payment**
You may want to see also

Qualifying events for COBRA include termination, reduction in hours, divorce, death, and Medicare eligibility
Qualifying events for COBRA are certain events that would cause an individual to lose health coverage under a group health plan. The type of qualifying event will determine who the qualified beneficiaries are and how long they will be entitled to COBRA coverage.
There are seven COBRA qualifying events that allow individuals to maintain their employer-sponsored health insurance:
- Termination of employment for reasons other than gross misconduct.
- Reduction in the number of work hours, affecting eligibility for health insurance.
- Transition between jobs, leading to a temporary loss of health insurance.
- Divorce or legal separation from the covered employee.
- The covered employee becoming entitled to Medicare.
- Death of the covered employee.
- Loss of dependent child status under the plan.
For covered employees, the only qualifying event is termination of employment (whether the termination is voluntary or involuntary) or reduction of employment hours. In that case, COBRA lasts for eighteen months.
If the qualifying event is the death of the covered employee, divorce or legal separation of the covered employee from their spouse, or the covered employee becoming entitled to Medicare, COBRA coverage for the spouse or dependent child lasts for 36 months.
The Perils and Pitfalls of Insurance: Understanding the Risks Covered by Your Policy
You may want to see also

COBRA coverage lasts for 18 or 36 months, depending on the scenario
The length of COBRA coverage depends on the nature of the qualifying event that made the individual eligible for it.
Employees are eligible for 18 months of continued coverage under COBRA if the qualifying event stems from a reduction of hours or termination of employment for reasons other than gross misconduct. Note that termination can be voluntary or involuntary, including retirement.
Employees who develop a disability, as determined by the Social Security Administration, within the first 60 days of receiving COBRA coverage are eligible for an additional 11 months of coverage, which equals a maximum coverage period of 29 months.
For other qualified beneficiaries — specifically, spouses and dependent children — the above durations also apply. However, these other qualified beneficiaries may be entitled to a maximum of 36 months of coverage if a second qualifying event occurs during the initial 18 months of coverage.
The second qualifying event cannot arise from termination of employment or reduction of hours. Instead, it must be due to the death of the covered employee, divorce or legal separation between the employee and their spouse, loss of dependent-child status under the plan rules, or the covered employee qualifying for Medicare.
In the state of New York, individuals are entitled to 36 months of continued health coverage at a monthly cost to them of 102% of the actual cost to the employer.
Understanding Hypnotherapy Insurance Billing for Better Reimbursement
You may want to see also

COBRA is a federal statute, and non-compliance can be reported to the U.S. Department of Labor
COBRA, the Consolidated Omnibus Budget Reconciliation Act, is a federal statute that provides continued health insurance coverage for employees who lose their jobs. It is applicable to employers with 20 or more full-time employees, requiring them to offer COBRA coverage to eligible workers and their dependents. The law ensures that individuals can maintain their previous health insurance plan, including prescription drugs, dental treatments, and vision care, albeit at a potentially higher cost.
Compliance with COBRA is crucial, and non-compliance can result in steep penalties and fines. The U.S. Department of Labor is responsible for ensuring compliance with COBRA, and employers who fail to adhere to its provisions can face legal issues and financial penalties. The Internal Revenue Service (IRS) enforces COBRA regulations, and non-compliance can result in excise tax penalties of $100 per day, per affected individual, amounting to a minimum of $2,500. Additionally, the Employee Retirement Income Security Act (ERISA) imposes statutory penalties of up to $110 per day for non-compliance.
The consequences of non-compliance with COBRA can be significant. Employees who are denied their rights under COBRA may file lawsuits, resulting in damages, interest, and attorney fees awarded to the plaintiffs. Class-action lawsuits associated with COBRA have led to substantial settlements for plaintiffs who successfully demonstrated systemic failures by employers to comply with COBRA notice requirements.
To avoid non-compliance issues, employers should understand their responsibilities under COBRA. They must provide written notification to covered employees and their dependents about their COBRA rights, maintain records demonstrating compliance, and promptly notify the plan administrator when a qualifying event occurs. By outsourcing COBRA administration to third-party administrators, employers can ensure compliance and mitigate the risks associated with non-compliance.
Unraveling the Complexities of Pregnancy Insurance Billing
You may want to see also
Frequently asked questions
COBRA, or the Consolidated Omnibus Budget Reconciliation Act, is a health insurance program that allows eligible employees and their dependents to continue receiving health insurance coverage when an employee loses their job or experiences a reduction in work hours.
The average monthly cost of COBRA insurance premiums ranges from $400 to $700 per individual. The cost of COBRA coverage is usually high because the newly unemployed individual has to pay the entire cost of the insurance (including the portion previously paid by the employer) plus an additional 2% in administrative fees.
To be eligible for COBRA insurance, you must meet three basic requirements: your group health plan must be covered by COBRA, a qualifying event must occur, and you must be a qualified beneficiary for that event. A qualifying event can include termination or a reduction of a covered employee's hours, divorce or legal separation from a covered employee, death of a covered employee, Medicare eligibility for a covered employee, or loss of a child's or dependent's health insurance coverage under the plan.
When a qualifying life event happens, you or your employer will notify the health plan. The plan will send an election notice that you will have 60 days to respond to. If you elect to take COBRA coverage, your employer may pay a portion of or the full amount of your insurance premium.