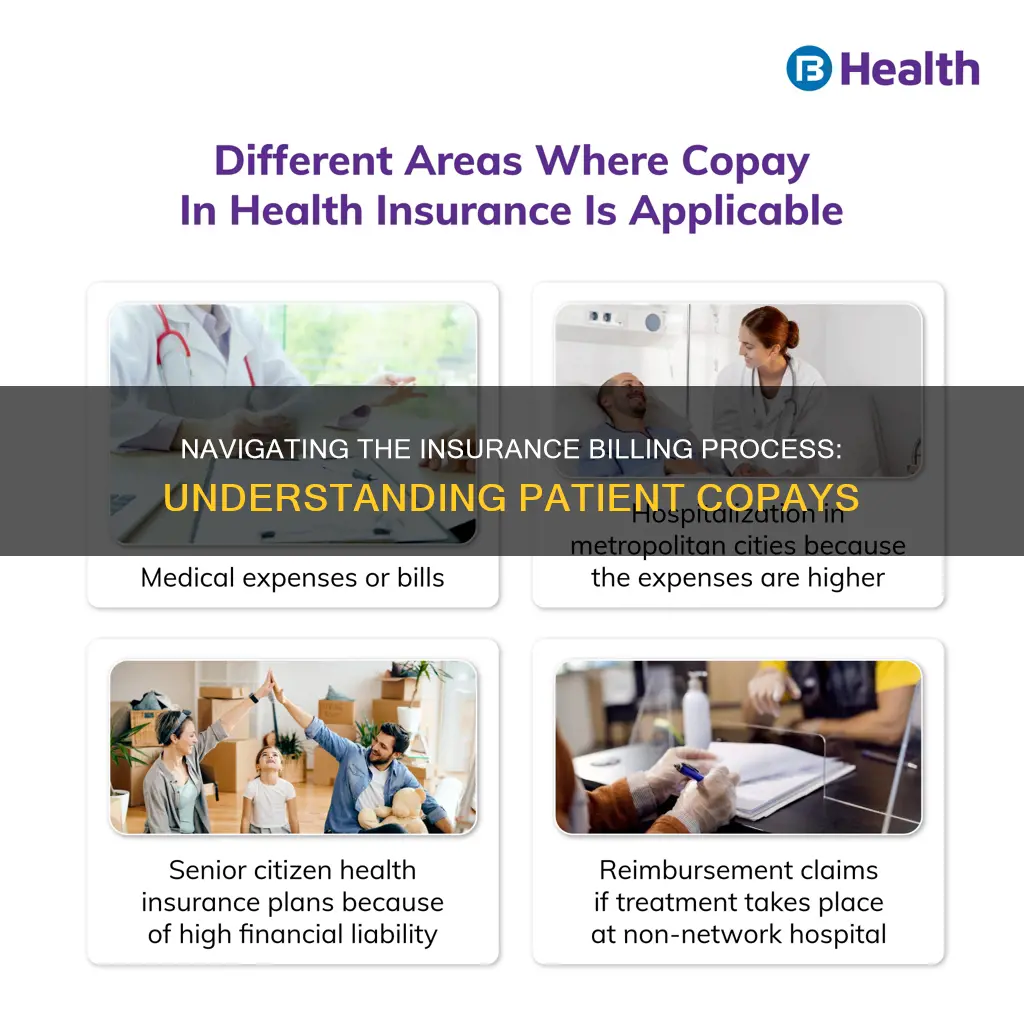
Billing insurance when a patient has a copay can be a confusing process. In general, insurance plans are a cost-sharing agreement between the patient and the insurance company. Many insurance companies cover the costs for preventive care, such as check-ups and vaccinations. For other services, insurance companies may require the patient to cover all costs until they reach a specified amount, known as a deductible. Once the patient reaches this amount, the insurance company starts paying for covered services. Copayments, or copays, are a fixed dollar amount that patients pay each time they receive medical care. For example, a patient with a $20 copay would pay $20 to the provider's office during a doctor's appointment. It's important to note that copay amounts can vary depending on the service provided. In addition to copays, patients may also be responsible for coinsurance, which is a percentage of the total cost of medical care. Understanding insurance terms and billing processes is crucial for both patients and healthcare providers to ensure accurate and transparent billing practices.
| Characteristics | Values |
|---|---|
| What is a copay? | A fixed dollar amount that you pay every time you receive medical care. |
| Example | If you have a $20 copay, you will need to pay $20 to the doctor's office every time you go in for an appointment. |
| Different copay amounts | Many plans have different copay amounts for different services. For example, your copay may be $20 for a checkup but $50 for a visit to an urgent care center. |
| Bill for copay | A bill for copay is not considered a surprise bill as it is expected. |
What You'll Learn

Understanding copayments, coinsurance, and deductibles
Copayments, coinsurance, and deductibles are all out-of-pocket costs for healthcare that you pay in addition to your monthly premium. However, the details of these costs vary by health plan.
Coinsurance
Coinsurance is the percentage of a medical charge that you pay, with the rest paid by your health insurance plan. This typically applies after your deductible has been met. For example, if you have 20% coinsurance, you pay 20% of each medical bill, and your health insurance will cover 80%.
Copay (or Copayment)
A copay is a set rate you pay for prescriptions, doctor visits, and other types of care. For example, you may have a $25 copay every time you see your primary care physician, a $10 copay for each monthly medication, and a $250 copay for an emergency room visit.
Deductible
A deductible is the set amount you pay for medical services and prescriptions before your coinsurance kicks in fully. For example, if you have a $1,000 deductible, you must pay $1,000 for your care out of pocket before your insurer starts covering a higher portion of costs. The deductible resets yearly.
Premium
The premium is the monthly payment you make to have health insurance. You pay the premium each month, even if you don't use the coverage. If you don't pay the premium, you may lose your insurance.
Out-of-Pocket Maximum
The out-of-pocket maximum is the limit of what you'll pay in one year, out of pocket, for your covered health care before your insurance covers 100% of the bill. The maximum out-of-pocket limit for marketplace health plans (those on the Affordable Care Act health insurance marketplace) is $9,450 for an individual and $18,900 for a family in 2024.
Understanding the Ins and Outs of Insurance Billing for Locum Tenens Assignments
You may want to see also

The No Surprises Act
Under the NSA, if you have private health insurance, you are protected from the most common types of surprise bills. The Act bans surprise bills for most emergency services, even if they are received out-of-network and without prior approval. It also bans out-of-network cost-sharing for most emergency and some non-emergency services, meaning you cannot be charged more than in-network cost-sharing for these services. Additionally, it bans out-of-network charges and balance bills for certain additional services, like anesthesiology or radiology, provided by out-of-network providers as part of a patient's visit to an in-network facility.
The NSA also establishes an independent dispute resolution process for payment disputes between health plans and providers. This process allows uninsured and self-pay individuals to dispute a medical bill if it is substantially greater than the good faith estimate they received from the provider. If you are insured and your health plan denies or partially denies a claim for service, you can appeal that decision.
The NSA provides protections for specific types of services in certain settings:
- Emergency Services: The NSA applies to most emergency services, including those provided in hospital emergency rooms, freestanding emergency departments, and urgent care centers licensed to provide emergency care. It also covers air ambulance transportation for emergency and non-emergency cases, but not ground ambulance services.
- Post-emergency Stabilization Services: The NSA defines emergency services to include post-stabilization services provided in a hospital following an emergency visit. Post-stabilization care is considered emergency care until a physician determines that the patient can be safely transferred to another in-network facility, and the patient must provide written consent to the transfer.
- Non-emergency Services at In-network Facilities: The NSA covers non-emergency services provided by out-of-network providers at in-network hospitals and other facilities. This includes situations where doctors who work in hospitals bill independently and do not participate in the same health plan networks.
To ensure compliance with the NSA, health plans and providers must notify consumers of their rights and protections under the Act. They must provide a one-page disclosure notice on a public website and give this disclosure to each patient receiving NSA-covered services. This notice must be provided no later than the date when payment is requested.
It's important to note that some providers can ask consumers to waive their rights under the NSA in specific circumstances. However, providers are never allowed to request a waiver for emergency services or certain other non-emergency services. Consent must be given voluntarily and cannot be coerced, although providers can refuse care if consent is denied.
The NSA is enforced by both federal and state agencies, depending on the type of health plan involved. The federal government has exclusive enforcement responsibility for most private health plans, while states lead enforcement for state-regulated plans.
Medigap and Supplemental Insurance: Understanding the Difference
You may want to see also

Cost-sharing
The monthly premiums you pay to get health insurance coverage aren't considered a type of cost-sharing. Cost-sharing comes into play when a policyholder uses medical and/or prescription drug insurance coverage.
The most common forms of cost-sharing are deductibles, copayments, and coinsurance. Copayments are set dollar amounts for covered services (e.g. $20 per general physician visit). Coinsurance is a percentage of the allowed cost for covered services (e.g. 20% of the allowed cost for a specialist visit). Deductibles are set dollar amounts that enrollees must pay before their plan starts to cover the service or a group of services (e.g. $200 drug deductible before drug coverage begins).
Understanding the Insurance Term Period: Unraveling the Fine Print
You may want to see also

Explanation of Benefits (EOB)
The Explanation of Benefits (EOB) is a document provided by the insurance company that breaks down the costs of a service or visit and outlines how much the patient is responsible for paying. It is important to understand the EOB as it provides valuable information about the patient's financial responsibility and coverage provided by their insurance plan.
The EOB will show the total amount billed by the healthcare provider and the amount that the insurance company will pay. It will also detail any discounts or adjustments made to the bill. Additionally, the EOB will specify the patient's copayment amount, deductible, and coinsurance, if applicable.
For instance, if a patient has met their deductible for the year, the EOB will indicate that the insurance company will cover a certain percentage of the costs, with the patient being responsible for the remaining percentage as coinsurance. On the other hand, if the patient has a copayment, the EOB will state the fixed dollar amount they need to pay for each visit or service.
It is important to note that the EOB is not a bill. Once the insurance company has processed the claim and determined the patient's responsibility, the healthcare provider will send a separate bill to the patient for the amount they owe. If patients have questions about their coverage or the amount covered by their insurance, they should contact their insurance company directly.
In addition to the EOB, patients have certain rights and protections under the No Surprises Act, which went into effect on January 1, 2022. This federal law protects patients with most types of health insurance from unexpected out-of-network medical bills in specific situations, such as emergency room visits, air ambulance services, and non-emergency care related to a visit to an in-network facility.
Understanding the Islamic Perspective on Term Insurance: Halal or Haram?
You may want to see also

State-specific regulations
New York
In New York, consumers are protected from surprise bills when treated by an out-of-network provider at a participating hospital or ambulatory surgical centre in their health plan's network. Additionally, if a participating doctor refers them to a non-participating provider, they are also protected from surprise bills. This protection also extends to emergency services in hospitals, including inpatient care following emergency room treatment.
If a patient receives a surprise bill, they are only required to pay their in-network cost-sharing amount (copayment, coinsurance, or deductible). If an out-of-network provider bills the patient for any amount above this, it is considered balance-billing, which is illegal in this situation.
Texas
In Texas, state law bans surprise bills from ground ambulance services if the patient has a state-regulated plan. A state-regulated plan is identified by having "DOI" (Department of Insurance) or "TDI" (Texas Department of Insurance) printed on the insurance card.
Federal Law
The No Surprises Act is a federal law that protects individuals from unexpected out-of-network medical bills. This includes emergency room visits, non-emergency care related to a visit to an in-network hospital or facility, and air ambulance services. This law applies to individuals with health insurance through an employer, the federal Health Insurance Marketplace, a State-based Marketplace, or other individual market coverage.
It is important to note that these regulations can vary by state and specific situations, so it is always advisable to refer to the relevant state laws and consult with legal or financial professionals for specific cases.
Unlocking the HMO Insurance Billing Process: A Comprehensive Guide
You may want to see also
Frequently asked questions
A copay, or copayment, is a fixed dollar amount that you pay every time you receive medical care. For example, if you have a $20 copay, you will need to pay $20 to the doctor's office each time you go in for an appointment.
After receiving care, the medical provider will send a bill to your insurance company. They will then determine how much they will pay for the service and how much you are responsible for. You will then receive a bill for the amount you owe, which will include your copay.
A deductible is a fixed dollar amount that you need to pay within a defined period, such as a year, before your insurance company starts covering some of the costs. With a copay, you pay a fixed amount each time you receive medical care, regardless of whether you have met your deductible.
Yes, you can still be billed for your copay even if you have insurance. This is not considered a surprise bill as it is an expected cost.
If you receive a bill that includes charges for your copay as well as other costs that should be covered by your insurance, you should contact your insurance company directly to clarify what is covered and what you are responsible for paying.