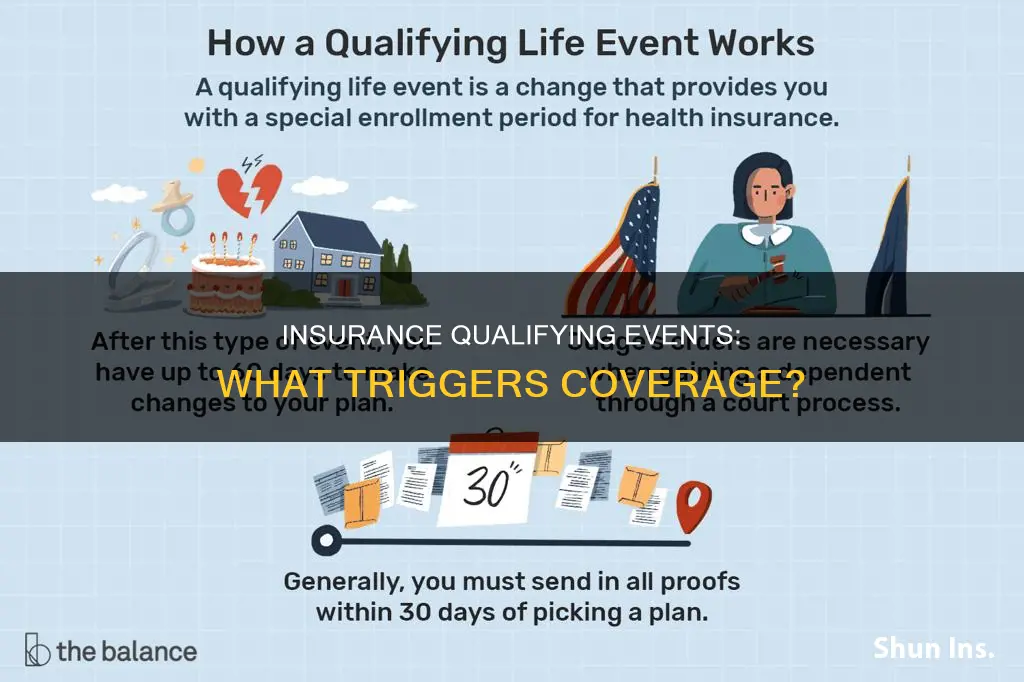
A qualifying life event (QLE) is a significant change in your life circumstances that allows you to alter your existing health insurance policy or sign up for a new one outside of the usual open enrollment period. These events can be planned or unexpected, but they must impact your personal or financial situation. Examples of qualifying life events include the birth or adoption of a child, marriage or divorce, the death of a spouse, a change in income, and the loss of existing health coverage. It's important to note that not all life-changing events are considered qualifying events, and specific documentation may be required to prove that a qualifying event has occurred.
| Characteristics | Values |
|---|---|
| Change in marital status | Getting married, divorced, or widowed |
| Family changes | Having a baby, adopting a child, or gaining a dependent |
| Loss of health coverage | Losing job-based, individual, or student health insurance plans |
| Loss of eligibility | Losing eligibility for Medicare, Medicaid, or CHIP |
| Age-related | Turning 26 and losing coverage through a parent's plan, or turning 65 |
| Changes in residence | Moving to a different ZIP code or county, moving to or from school, or moving to transitional housing |
| Income changes | Changes in income that affect the coverage you qualify for |
| Citizenship status | Gaining U.S. citizenship or becoming a lawfully present resident |
| Legal status | Leaving incarceration, or gaining status as an Alaska Native Claims Settlement Act (ANCSA) Corporation shareholder |
What You'll Learn

Birth or adoption of a child
The birth or adoption of a child is a major life event that can affect a person's health insurance needs. This is considered a qualifying life event that allows individuals to purchase or make changes to their health plan outside of the annual Open Enrollment Period. This is applicable to ACA-compliant major medical plans, including individual market, small group, and large group insurance plans.
When a child is born or adopted, the parents are given a special enrollment period to adjust their health insurance plan. This period typically lasts 60 days, starting from the date of birth or adoption. During this time, parents can add the new family member to their existing plan or make changes to their current coverage to ensure the child's health needs are met. It is important to note that the coverage for the child is typically back-dated to the date of birth or adoption, although parents may also have the option to select a later effective date.
To enrol the child in the insurance plan, parents may be required to provide certain documents as proof of the qualifying life event. These documents typically include birth certificates or adoption records. By submitting these documents within the specified timeframe, parents can ensure that their child is covered under their health insurance plan without any gaps in coverage.
In addition to the birth or adoption of a child, other qualifying life events that trigger special enrollment periods include marriage, divorce, loss of other health coverage, permanent moves to a different area, and changes in income that affect subsidy eligibility. These events allow individuals and families to make necessary adjustments to their health insurance plans to accommodate their changing needs.
Understanding Transamerica's Annual Renewable Term Life Insurance: Flexibility and Protection
You may want to see also

Death of a spouse
The death of a spouse is a qualifying event for insurance, allowing the surviving spouse to make changes to their health insurance plan. This is classified as a "change in household" or "loss of health coverage", which are two of the four basic types of qualifying life events.
Changes in Household
The death of a spouse constitutes a change in household, as the size of the household is changing, and coverage must be adjusted to reflect this change. This type of qualifying life event also includes getting married, divorced, or legally separated.
Loss of Health Coverage
The death of a spouse can also result in a loss of health coverage, especially if the deceased spouse was the primary holder of the family's health insurance policy. In this case, the surviving spouse may be able to purchase their own individual plan through a Special Enrollment Period (SEP).
Special Enrollment Period
A Special Enrollment Period is a window of time when people can enroll in health insurance outside of the Open Enrollment Period. It is triggered by a qualifying life event, such as the death of a spouse, and allows the surviving spouse to make necessary updates to their health insurance coverage. The length of the special enrollment period can vary, but it is generally 30-60 days before or after the qualifying event.
Documentation
To make changes to a health insurance plan after the death of a spouse, the surviving spouse may need to provide certain documentation. This typically includes a death certificate and proof of prior coverage within the last 60 days. It is important to notify the health insurance provider as soon as possible to determine eligibility and understand any specific documentation requirements.
Term Insurance: Navigating the Purchase Process with Confidence
You may want to see also

Change in marital status
A change in marital status is a qualifying life event that can impact your insurance in several ways. Firstly, if you get married, you can apply to extend your insurance coverage to include your spouse. This typically involves changing your level of coverage from single to family or couple's coverage. On the other hand, if you are going through a divorce, you may need to remove your spouse from your insurance policy.
In terms of health insurance, a change in marital status can trigger a Special Enrollment Period, allowing you to enroll in health insurance or make changes to your existing plan outside of the regular annual Open Enrollment Period. For example, if you recently got married, you may want to add your spouse to your health insurance plan. Similarly, if you are going through a divorce, you may need to remove your spouse from your health insurance and find a new plan as a single individual.
It's important to note that the impact of a change in marital status on insurance rates varies depending on your location and insurance provider. In some provinces or states, your marital status may be used as a factor in determining your insurance rate. For example, in Ontario, Canada, car insurance companies use marital status as part of their risk assessment profile when setting rates. On the other hand, in provinces like Manitoba and British Columbia, insurance companies do not consider marital status when determining auto insurance rates.
To update your insurance coverage due to a change in marital status, you may need to provide relevant documentation, such as a marriage license or divorce papers. It's recommended to notify your insurance provider as soon as possible about any changes in your marital status to ensure you have the necessary coverage and to understand any potential impact on your insurance rates.
Rethinking Insurance in America: A Comprehensive Reform for a Secure Future
You may want to see also

Loss of health coverage
Types of Coverage Loss
There are several ways in which an individual can lose their health coverage, including:
- Losing existing health coverage, such as job-based, individual, or student plans.
- Losing eligibility for Medicare, Medicaid, or the Children's Health Insurance Program (CHIP).
- Turning 26 and losing coverage through a parent's plan.
Special Enrollment Period
When an individual loses their health coverage, they are given a Special Enrollment Period to enroll in a new health plan. This period typically lasts 60 days, beginning 60 days before the existing plan's termination date and continuing for 60 days after it ends. This allows individuals to enroll in a new plan without any gap in coverage, as long as their old plan ends on the last day of the month.
If an individual enrolls in a new plan before the date their old plan ends, the effective date of the new plan will be the first of the month following the loss of coverage. However, if the old plan ends mid-month, some exchanges allow the new coverage to take effect on the first day of the month in which the old coverage will end, as long as the individual applies before the first day of that month. This results in a partial month of overlapping coverage.
Minimum Essential Coverage
It is important to note that the coverage that is lost must be considered minimum essential coverage. Short-term plans, for example, are not considered minimum essential coverage, so losing this type of plan does not qualify as a loss of coverage. However, there are exceptions to this rule, such as losing pregnancy-related Medicaid coverage, CHIP unborn child coverage, or Medically Needy Medicaid.
Adjusting Your Auto-Payments with Erie Insurance: A Step-by-Step Guide
You may want to see also

Change in residence
Changes in residence are considered qualifying life events (QLEs) for insurance. Moving to a new address can impact your health insurance coverage, and you may need to update your plan to ensure you have access to healthcare services in your new location.
To be considered a qualifying life event, a change in residence typically needs to result in a change in your health plan area or service area. This means that moving to a different ZIP code or county can be a qualifying event, as you may need to switch to a new health plan with providers in your new area. It is important to notify your health insurance provider as soon as possible about your change in residence to determine your eligibility for a qualifying life event and understand your options for updating your coverage.
There are several specific scenarios related to changes in residence that are considered qualifying life events:
- Moving to a different ZIP code or county: If you move to a new ZIP code or county that is outside of your current health plan's service area, you may need to switch to a new plan with providers in your new location.
- Students moving to or from their place of study: Students who move to attend school or return home from their studies may experience a change in their health coverage needs and may be eligible for a qualifying life event update to their insurance plan.
- Seasonal workers moving to or from their work location: Similar to students, seasonal workers who move to their work location or return home after the season ends may need to adjust their health plan accordingly.
- Moving to or from a shelter or transitional housing: Transitional housing may have different health coverage options, and moving in or out of such housing may trigger a qualifying life event.
- Moving to the US from a US territory or foreign country: Individuals moving to the US from another country or a US territory may need to enrol in a new health plan to ensure they have access to healthcare services in their new location.
It is important to note that not all changes in residence may be considered a qualifying life event. For example, if you move within the same health plan service area, it may not be considered a qualifying event. Additionally, you may need to provide documentation, such as proof of residency from your new and old addresses, to support your request for a plan change due to a change in residence.
SIBO: A Disease or Not?
You may want to see also
Frequently asked questions
Qualifying events for insurance are significant life-changing situations that allow you to alter an existing health insurance policy or sign up for a new one outside of the annual open enrollment period.
Examples of qualifying events include the birth or adoption of a child, marriage, divorce, death of a spouse, and changes in employment status.
If you experience a qualifying life event, you will likely qualify for a Special Enrollment Period, which allows you to enroll in a health plan outside of the regular annual open enrollment period.
After experiencing a qualifying event, notify your health insurance provider as soon as possible and provide any necessary documentation. You typically have 30 to 60 days to make changes to your health insurance plan.